Otology
Vol. 44: Issue 6 - December 2024
Factors influencing audiologic outcomes in ossiculoplasty for chronic otitis media: a prospective multicentre study
Abstract
Objective. Chronic otitis media (COM) is a prevalent condition affecting auditory function. Ossiculoplasty is a known treatment strategy, but its effectiveness concerning the presence of cholesteatoma has not been extensively studied.
Methods. We conducted a multicentre study involving 153 patients diagnosed with COM without cholesteatoma (ncCOM) and with cholesteatoma (cCOM). Patients underwent ossiculoplasty, and postoperative hearing outcomes were analysed.
Results. After patient selection, 133 participants were included. Postoperatively, significant improvements in hearing function were observed in both groups, substantiating the role of ossiculoplasty in treatment of COM. However, different outcomes were noted between ncCOM and cCOM. Patients with cCOM demonstrated a slightly lesser degree of hearing improvement post-surgery compared to their ncCOM counterparts.
Conclusions. Our findings confirm ossiculoplasty as a standard and effective treatment strategy for COM. The presence of cholesteatoma may influence the effectiveness of surgery, underscoring the need for individualised surgical planning. Future research should focus on confirming these results and more comprehensively exploring the impact of cholesteatoma on surgical outcomes.
Introduction
Ossiculoplasty (OPL) is a surgical procedure designed to reconstruct the middle ear’s conductive mechanism when the ossicular chain is compromised due to a middle ear pathology. Typically performed during tympanoplasty (TPL), OPL may occasionally be postponed to a secondary operation 1. The goal of OPL is to create a durable and stable connection between the natural or reconstructed tympanic membrane and the labyrinthine fluids – this connection does not necessarily pass through the oval window – utilising either biological or artificial prostheses 2. Concurrently, TPL aims to restore the middle ear cavity’s integrity, eradicate disease definitively, reconstruct the tympanic membrane when needed, and enhance the conductive hearing that was previously impaired 3. Ossicular erosion, a common consequence of chronic otitis media (COM), often necessitates OPL, especially when the incus long process, stapes crura, incus body, or the malleo-incudal and incudo-stapedial joints are compromised 4. The erosive process is typically more aggressive in cholesteatoma due to the enzymatic activity of its proliferative epithelium. Moreover, surgery for COM can be a source of conductive hearing loss by introducing ossicular discontinuity, often necessitating partial or complete removal of the ossicular chain 5. OPL is a complex procedure with multiple surgical options: choosing between a partial ossicular replacement prosthesis (PORP) and a total ossicular replacement prosthesis (TORP), deciding on a microscopic versus endoscopic approach, and selecting the type of prosthesis 6,7. The decision to use a PORP or a TORP is contingent upon the condition of the stapes superstructure, mirroring the decision-making process in stapes surgeries for otosclerosis 8. Literature data suggests a 5-year success rate of 66% for PORP and 33% for TORP 5-8. Regarding materials for prosthesis, the choice should prioritise biocompatibility and mechanical similarity to the natural ossicular system. While not as common, malleus reconstruction follows the same criteria. Alternatively, autologous cartilage from the tragus or concha is readily available and poses no risk of disease recurrence 5. These off-the-shelf prostheses come in various sizes and shapes, reduce duration of surgery and risk of recurrence, but are prone to extrusion and displacement. Comparative studies have evaluated the auditory outcomes of biological versus synthetic prostheses 4-8, but a combination of both materials can also be used. The success of the surgery may be influenced by several factors such as functioning eustachian tube, an aerated middle ear cavity and the presence of otorrhoea 3,7,8. Much of the literature on OPL comprises small, retrospective case series from single institutions, which limits the data’s generalisibility and statistical significance. The dearth of high-quality evidence has made it difficult for systematic reviews to establish conclusive findings, highlighting the urgent need for prospective, multicentre trials with standardised protocols. Our research seeks to bridge this knowledge gap through an extensive, collaborative study spanning multiple facilities and geographic areas. By tapping into our network of otologic surgery practices, we have gathered a significant cohort of OPL patients, which will contribute to addressing the existing deficiencies in current knowledge.
Materials and methods
Study design
This investigation was designed as a prospective, controlled, and longitudinal study. The study protocol is summarised in Figure 1. It was conducted in accordance with the strengthening the reporting of observational studies in epidemiology (STROBE) and consolidated standards of reporting trials (CONSORT) guidelines 9. The study period spanned three years, from January 2021 to December 2023, allowing for a comprehensive investigation. The surgical approach and technique used in this study were consistent with the recommendations outlined in the European Academy of Otology and Neurotology (EAONO)/Japanese Otological Society (JOS) Consensus Statement on the definitions and classification of middle ear surgery 10. Mastoidectomy procedures were categorised as either canal wall up (CWU) or canal wall down (CWD) based on the International Otology Outcome Group (IOOG) classification 11, depending on whether the posterior canal wall was preserved or removed during surgery. Six different centres were included in the analysis: San Luigi Gonzaga Hospital, Policlinic Umberto I, Morgagni Pierantoni Hospital, Hospital Gravina e Santo Pietro, Vicenza Civil Hospital, and Policlinic G. Rodolico.
Patient selection
The target population for this study was individuals diagnosed with COM from 18 to 65 years old. A total of 20 patients was required from each of the 6 centres participating in the analysis, with an equal distribution between the non-cholesteatomatous chronic otitis media (ncCOM) and chronic otitis media with cholesteatoma (cCOM) groups. The participants received an average follow-up period of at least 1 year after surgery. The presence or absence of cholesteatoma was confirmed through clinical examination and imaging. The study recruited only acquired cholesteatoma. Patients of all ages and genders were included to ensure a diverse study population. Several exclusion criteria were established to control for potential confounding variables. Firstly, patients diagnosed with other otologic diseases, such as Meniere’s disease, otosclerosis, or acute otitis media, were excluded. Similarly, patients with systemic diseases that could influence hearing, such as diabetes mellitus, autoimmune disorders, or conditions requiring ototoxic medications, were also excluded. Patients who had previously undergone otologic surgery, who were unable or unwilling to give informed consent, or unable to follow the study procedures due to cognitive or other impairments were also excluded. The follow-up program included frequent visits in the first year after OPL surgery, with comprehensive evaluations scheduled at 1, 3, 6, and 12 months after surgery to closely monitor anatomic and functional outcomes.
Statistical analysis
Independent t-tests were employed for continuous variables like age and duration of hearing loss, whereas Chi-square tests were used for categorical variables such as gender and smoking status. Pure tone audiometry (PTA) was assessed preoperatively and at each control visit to evaluate the functional results. Hearing outcomes were primarily evaluated using air-bone gap (ABG) measurements, which were taken both pre- and postoperatively. The frequencies used to obtain the ABG in hearing tests were 500 Hz, 1000 Hz, 2000 Hz and 4000 Hz. We considered an ABG ≤ 20 dB as functional success. The change in ABG (ΔABG) was then calculated for each patient. To explore the relationship between a single dependent variable and several independent variables, a multiple regression analysis was performed. We searched for factors significantly related to ΔABG among the recorded variables, quantifying the relationship and evaluating their predictive ability in each group of patients.
The multiple regression equation used in this study was: ΔABG = β0 + β1(age) + β2 (period of hearing loss) + β3 (hearing loss type) + β4 (otorrhoea) + β5 (site of perforation) + β6 (ossicular chain status) + β7 (material of OPL) + β8 (surgeon) + β9 (postoperative complications). The postoperative complications included wound infection, bleeding and prosthesis extrusion, which were observed and recorded for each patient. The regression squared (R-squared) and adjusted R-squared values were evaluated to quantify the proportion of variance in ΔABG for the regression model. A p-value < 0.05 was considered statistically significant. All statistical analyses were performed using a statistical software package (IBM SPSS Statistics for Windows, IBM Corp. Released 2017, Version 29.0 Armonk, NY: IBM Corp).
Results
This study involved 133 patients diagnosed with COM, 73 with ncCOM and 60 with cCOM (Fig. 2). There were 70 females and 63 males; the right ear was affected in 60 patients and the left ear in 73. Otorrhoea was present in 113 patients. In the ncCOM group, females were more prevalent (63%), whereas in the cCOM group, males were slightly more common (60%) (p = 0.01). Lifestyle factors such as smoking status did not show significant differences between the two groups (p = 0.811). Similarly, the duration of hearing loss did not significantly differ between patients with COM with or without cholesteatoma (p = 0.471). Clinical manifestations such as otorrhoea did not differ substantially between the two groups (p = 0.314), while ossicular chain status was significantly different between groups (p = 0.02), as was the site of eardrum perforation (p < 0.001). Differences were noted in the type of OPL performed, with PORP being more common in the ncCOM group and TORP in the cCOM group (p = 0.001). The choice of OPL material also differed significantly. Postoperative complications did not significantly differ overall between groups (p = 0.051). However, it is worth noting certain complications were specific to the cCOM group as summarised in Table I.
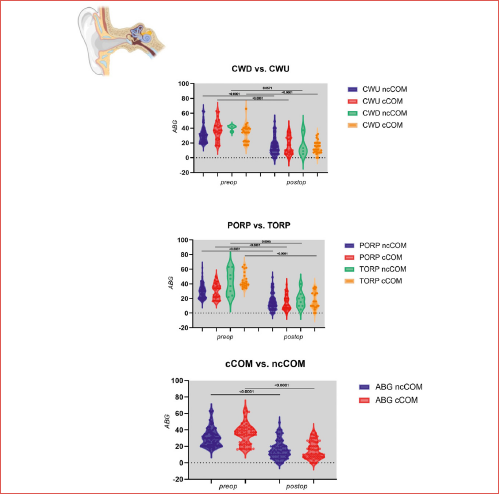
ncCOM vs cCOM
The mean preoperative ABG was slightly higher in the cCOM group (35.4 ± 12.5 dB) compared to the ncCOM group (31.2 ± 11.3 dB). This difference was statistically significant (p = 0.044; Fig. 3). The postoperative ABG was similar in both groups (ncCOM 15.9 ± 11.1 dB vs cCOM 15.1 ± 10.5 dB; p = 0.701). The change in the ABG from preoperative to postoperative was slightly higher in the cCOM group than in the ncCOM group (20.2 ± 14.9 dB vs 15.2 ± 13.5 dB; p = 0.048; Table II). While there were significant differences in preoperative ABGs and the change in ABG values between groups, there were no significant differences comparing these values between the types of mastoidectomy within each group. Among the 61 ncCOM patients who underwent CWU mastoidectomy, the preoperative ABG was 31.4 ± 11.4 dB, the postoperative ABG was 15.8 ± 11.49 dB, and the change in ABG was 15.5 ± 13.7 dB, while the 4 CWD patients reported a greater change in ABG of 24.5 ± 13.1 dB (Fig. 4). None of the intergroup comparisons for CWD and CWU mastoidectomy in the ncCOM group were statistically significant (p = 0.119, p = 0.980, and p = 0.213, respectively). The differences in preABG, postABG, and ΔABG between CWU and CWD mastoidectomy in the cCOM group were not statistically significant (p = 0.212, p = 0.330, and p = 0.661, respectively).
Prosthesis type and audiology outcomes
Considering the type of prosthesis used in patients with ncCOM, significant differences in preoperative ABG were observed (p = 0.002). However, the postoperative PORP and TORP comparison of ABG outcomes was not statistically significant (p = 0.514), and a near-significant trend was observed among ΔABG comparison (p = 0.05; Figure 5). A similar trend was observed in the cCOM group, with a more pronounced difference in preoperative ABG for PORP than for TORP (p < 0.001), with no differences in postoperative findings (p = 0.265). When considering ΔABG, a notable difference was observed for PORP (16.1 ± 12.6 dB) compared to TORP (27.8 ± 15.9 dB; p < 0.001; Table II).
Multiple regression analysis
In regression analysis for the ncCOM group, the R-squared was 0.376. However, after adjusting for the number of predictors, the adjusted R-squared value decreased to 0.354. The majority of variables were not significant predictors within the model. Only the presence of otorrhoea (F = 7.616, p < 0.001) and condition of the ossicular chain (F = 4.737, p < 0.001) emerged as significant predictors. In contrast, patient age at intervention (F = 1.627, p = 0.079), duration of hearing loss (F = 1.436, p = 0.147), site of perforation (F = 1.191, p = 0.308) and OPL material (F = 1.519, p = 0.113) were not significant predictors within the model. Complications demonstrated the least significance in this group (F = 0.627, p = 0.919) (Tab. III). In the multiple linear regression analysis conducted for the cCOM group, the model’s R-squared was 0.583. However, when the number of predictors was accounted for the adjusted R-squared value decreased to 0.569. Several variables were significant predictors of ABG, such as age (F = 2.303; p = 0.014), hearing loss prior to intervention (F = 4.391; p < 0.001), and otorrhoea (F = 3.733; p < 0.001). The perforation site in the tympanic membrane similarly held significance (F = 4.063; p < 0.001). The condition of the ossicular chain, which plays a crucial role in sound conduction, was also identified as a significant predictor (F = 2.547, p < 0.001) as was the choice of reconstruction material (F = 2.796; p = 0.004). Complications was the variable with the highest significance (F = 38.91; p < 0.001).
Discussion
Numerous elements have the potential to impact restoration of the ossicular chain. In treating individuals with COM, achieving satisfactory functional outcomes relies on skillful ossicular reconstruction and the specific conditions and context in which the surgery occurs. Indeed, favourable results appear to be more attainable when confronted with a well-maintained middle ear mucosa and a ”dry” ear. In contrast, factors such as ear drainage, granulomatous conditions in the middle ear, otitis media with effusion, and cholesteatoma may diminish the likelihood of a successful functional recovery 12,13. In this investigation, we conducted a thorough analysis of the impact of ossiculoplasty in patients with COM, with a specific emphasis on the potential influence of cholesteatoma at the time of initial diagnosis on functional recovery. Our findings contribute valuable insights into the comprehension and treatment of these conditions. The inclusivity of our patient cohort, spanning various ages and sex, enhances the applicability of our conclusions to a diverse demographic. The results notably revealed substantial differences in auditory outcomes between patients with ncCOM and those with cCOM; specifically, a higher ΔABG was evident in the cCOM group compared to the ncCOM. This observation implies that the presence of cholesteatoma might impact the outcomes of ossiculoplasty, possibly attributed to the often more extensive middle ear involvement associated with this pathology.
The mean preABG value was 30.1 ± 10.2 dB for the cCOM group and 29.8 ± 9.8 dB for the ncCOM group in the context of TORP following CWU (p < 0.001). Other surgical subgroups followed this trend, with the cCOM group exhibiting noticeably higher preABG values. Interestingly, the difference in the postoperative aero-osseous gap (postABG) was still statistically significant (p < 0.001 for TORP with CWU), even though the cCOM group demonstrated a greater improvement (mean ΔABG of 16.1 ± 12.6 dB for cCOM with TORP and CWU vs 14.2 ± 12.6 dB for ncCOM with TORP and CWU). This pattern was consistent across all surgical subgroups and suggests that while patients with cholesteatoma can benefit from surgery to enhance their hearing, the condition may restrict their potential for improvement compared to patients without cholesteatoma. Our findings could be used to forecast the likelihood that patients having total ossicular repair will have better hearing, which has important implications for clinical practice.
While analogous findings are present in the literature 14,15, establishing a direct correlation between cholesteatomatous pathology and auditory outcomes following ossiculoplasty requires further elucidation. Furthermore, it is crucial to highlight that our study underscored the efficacy of ossiculoplasty in enhancing hearing outcomes for individuals with COM, irrespective of the presence of cholesteatoma. These findings advocate for incorporating ossiculoplasty as a standard procedure in the therapeutic strategy for these patients. Nevertheless, a personalised surgical strategy is paramount, considering that the type of ossiculoplasty and the materials employed can influence the postoperative results. The management of cCOM has undergone significant transformations, transitioning from radical mastoidectomy to tympanoplasty with or without ossiculoplasty 16-19. CWU was the predominant procedure for many years, offering improved hearing outcomes; however, it was associated with higher recurrence rates than CWD, often necessitating multiple surgical interventions 20,21. Hence, the preferred approach for middle-ear cholesteatoma is considered to be CWD 22,23. While this procedure is now commonly performed, literature documenting hearing outcomes is scarce and conflicting 22-26. Ossiculoplasty in CWD is not extensively addressed in the current literature, and the wide variability frequently influences functional results in surgical techniques. Retrospective analysis of the postoperative hearing results from 126 primary patients with cholesteatoma undergoing one-stage ossicular restoration with intact and movable stapes was conducted by Acke et al. 27. The best results for hearing were obtained with incus interposition in closed cavity procedures. However, open cavity surgery should not be avoided purely for reasons related to hearing, as postoperative ventilation and the severity of the disease may also have an impact on hearing outcomes.
In our investigation, we observed no significant statistical variance in hearing outcomes between patients who underwent CWU and those who underwent CWD mastoidectomy in both study groups. Concerning the choice between PORP and TORP, noticeable variations in the impact on the hearing of patients with COM were evident. While the literature does not consistently support this observation 15-20, with some studies indicating that the presence of the stapes superstructure may not significantly influence hearing outcomes, this research highlights the crucial role of meticulous selection of a surgical approach that is tailored to the distinct pathology. In addition, results may change when considering new ossicular reconstruction techniques that have been tested. Esser et al. reviewed the results of a surgical technique employing a modified TORP as a PORP between the footplate and incus 28. The ossiculoplasty procedure was safe and successful for the treatment of isolated stapes superstructure abnormalities.
The comprehensive statistical analysis conducted in this study enabled us to identify factors influencing the variation in air-bone gap (ΔABG). Among patients with ncCOM, only otorrhoea and the condition of the ossicular chain at the time of surgery demonstrated an impact on the gap variation. The scenario was more intricate in the group of patients with cCOM, where nearly all factors considered exhibited some influence on ΔABG, with a greater weight associated with the presence of potential complications (such as prosthesis extrusions or neotympanic perforations). These findings may aid in predicting postoperative outcomes and tailoring treatment plans to the individual needs of patients. However, an important factor in the choice of treatment is the cost benefits of surgery, the possibility of recurrence, and the impact on health care spending. Lewis et al. conducted a registry study in western Sweden between 2014 and 2018, examining the costs and health care utilisation related to COM in 656 adult patients undergoing middle ear surgery 29. The findings revealed that over the course of the 5-year period, the subjects had 13,782 healthcare contacts at a total cost of SEK 61.1 million (EUR 6 million). The most expensive quartile of subjects accounted for 60% of the total costs, primarily from inpatient ENT care and revision surgeries. These findings suggest that, in challenging cases where revision ossiculoplasty is likely, alternative options like implants or hearing aids should be taken into consideration, particularly when the only reason for further surgery is to improve hearing.
Study limitations
Despite providing valuable insights, it is crucial to recognise the limitations of our study. Our study was conducted as a multicentre investigation, and due to potential variations in surgical techniques and patient demographics, the results may not be universally applicable to other settings. The exclusion of patients with other otologic or systemic diseases could limit the generalisability of our results to these specific patient populations. Such selective criteria, while necessary to control for confounding variables, might affect the external validity of our findings. The brief follow-up period of one year, which might not adequately capture the recurrence and long-term progression of nc/cCOM, was another weakness of this study. This short time period could miss issues that develop later on or late recurrences that happen after the study’s end. Moreover, while its longitudinal design offers valuable long-term data, it may also introduce certain biases. These could include loss to follow-up or the impact of unmeasured confounding variables over time.
Furthermore, ΔABG, for each audiometric frequency under consideration would be fascinating and maybe instructive. With more detailed information, treatment plans might be more precisely tailored and patient outcomes could be enhanced, offering deeper insights into the unique hearing outcomes and differences across different frequencies. Nevertheless, this comprehensive frequency-specific analysis was absent from the current study, which is another shortcoming that might be addressed in future research.
Conclusions
Our multicentre study provides an in-depth analysis of the impact of ossiculoplasty on hearing outcomes for patients with COM with and without cholesteatoma. The results affirm ossiculoplasty as a reliable and effective treatment strategy for these conditions, demonstrating significant improvements in postoperative hearing. The differing outcomes observed between ncCOM and cCOM patients highlight the need for personalised surgical planning, considering the potential influence of cholesteatoma. Moving forward, additional research should aim to confirm and expand on these findings. Detailed examination of the effects of cholesteatoma on surgical outcomes would be worthwhile, as would the identification of other potential predictors of hearing improvement. Furthermore, research into refining ossiculoplasty techniques and materials could lead to even better patient outcomes.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
GF, AM: conceptualisation; PC: methodology; FM: software; AP, GA, CG: validation; GC, GM: formal analysis; SM: investigation; AP, MDL: resources; SR, AM: data curation; AM, GF: writing – original draft preparation; GI: writing – review and editing; SF: visualisation; AM: supervision; GF: project administration. All authors have read and agreed to the published version of the manuscript.
Ethical consideration
This study was approved by the San Luigi Ethical Committee, Turin) (Protocol number: 3/2023). The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki. Written informed consent was obtained from each participant/patient for study participation and data publication.
History
Received: February 17, 2024
Accepted: May 29, 2024
Figures and tables
Figure 1. Flow-diagram of the study protocol.
Figure 2. Evaluation of preoperative and postoperative outcomes for partial ossicular reconstruction prosthesis (PORP) versus total ossicular reconstruction prosthesis (TORP). The results demonstrate the effectiveness of both surgical approaches in addressing hearing loss in patients with distinct middle ear pathologies.
Figure 3. Analysis of preoperative and postoperative air-bone gap (ABG) outcomes for patients with non-cholesteatomatous (ncCOM) and cholesteatomatous chronic otitis media (cCOM). The data highlight significant differences in hearing improvement between the two groups.
Figure 4. Comparison of chronic otitis media (COM) with and without cholesteatoma. This figure illustrates the impact of surgical interventions of CWD vs CWU on hearing outcomes in patients with different tympanic membrane conditions.
| Parameter | ncCOM (N = 73) | cCOM (N = 60) | p value |
|---|---|---|---|
| Age | 47.8 ± 16.9 | 43.9 ± 23 | 0.259 |
| Sex | |||
| Female | 46 (63%) | 24 (40%) | |
| Male | 27 (37%) | 36 (60%) | |
| 0.010 | |||
| Smoking | |||
| Smokers | 45 (62.6%) | 40 (66.7%) | |
| Non-smokers | 27 (37%) | 19 (31.7%) | |
| Former-smokers | 1 (1.4%) | 1 (1.6%) | |
| 0.811 | |||
| Duration of hearing loss | |||
| < 1 year | 36 (49.3%) | 27 (45%) | |
| 1-3 years | 27 (37%) | 28 (46.7%) | |
| > 5 years | 10 (13.7%) | 5 (8.3%) | |
| 0.471 | |||
| Otorrhoea | |||
| Present | 64 (87.7%) | 49 (81.7%) | |
| Not present | 9 (12.3%) | 11 (18.3%) | |
| 0.314 | |||
| Side | |||
| Right | 32 (43.8%) | 28 (46.7%) | |
| Left | 41 (56.2%) | 32 (53.3%) | |
| 0.825 | |||
| Type of MPL | |||
| Underlay | 68 (93.2%) | 50 (83.3%) | |
| Overlay | 5 (6.8%) | 9 (15%) | |
| 0.119 | |||
| Material of MPL | |||
| Fascia | 61 (83.6%) | 49 (81.7%) | |
| Cartilage | 5 (6.8%) | 2 (3.3%) | |
| Fascia + cartilage | 7 (9.6%) | 8 (13.3%) | |
| 0.552 | |||
| Type of OPL | |||
| PORP | 65 (89%) | 39 (65%) | |
| TORP | 8 (11%) | 21 (35%) | |
| 0.001 | |||
| Material of OPL | |||
| Incus | 16 (21.9%) | 6 (10%) | |
| Malleus | 5 (6.8%) | 8 (13.3%) | |
| Cartilage | 12 (16.4%) | 20 (33.3%) | |
| Titanium | 3 (4.1%) | 4 (6.7%) | |
| Hydroxyapatite | 37 (50.7%) | 22 (36.7%) | |
| 0.034 | |||
| Surgical procedure | |||
| Type I tympanoplasty | 8 (11%) | 0 | |
| Canal wall up | 61 (83.6%) | 34 (56.7%) | |
| Canal wall down | 4 (5.5%) | 26 (43.4%) | |
| < 0.0001 | |||
| Ossicular chain | |||
| Hypomobile | 11 (15.1%) | 7 (11.7%) | |
| Erosion of incus | 15 (20.5%) | 19 (31.7%) | |
| Absence of incus | 40 (54.8%) | 19 (31.7%) | |
| Erosion of the stape | 3 (4.1%) | 2 (3.3%) | |
| Absence of the stape | 4 (5.5%) | 13 (21.7%) | |
| 0.02 | |||
| Site of perforation | |||
| Absent | 3 (4.1%) | 0 | |
| Posterior | 6 (8.2%) | 1 (1.7%) | |
| Anterior | 28 (38.4%) | 4 (6.7%) | |
| Epytympanic/superior | 10 (13.7%) | 31 (51.7%) | |
| Inferior | 3 (4.1%) | 6 (10%) | |
| Subtotal | 9 (12.3%) | 12 (20%) | |
| Total | 14 (%) | 6 (10%) | |
| < 0.0001 | |||
| Complications | |||
| None | 66 (90.4%) | 53 (88.3%) | |
| Dysgeusia | 5 (6.8%) | 1 (1.7%) | |
| Prosthesis dislocation | 3 (4.1%) | 0 | |
| Prosthesis extrusion | 2 (2.7%) | 1 (1.7%) | |
| Neotympanum perforation | 0 | 4 (6.7%) | |
| 0.051 | |||
| Hearing levels (preoperative) | |||
| Mild (≤ 40 dB) | 21 (28.8%) | 8 (13.3%) | |
| Moderate (41-70 dB) | 47 (64.4%) | 42 (70%) | |
| Severe (> 70 dB) | 5 (6.8%) | 10 (16.7%) | 0.005 |
| Legend: OPL: ossiculoplasty; PORP: partial ossicular reconstruction prosthesis; TORP: total ossicular reconstruction prosthesis; ncCOM: non colesteathomatous chronic otitis media; cCOM: colesteathomatous chronic otitis media; MPL: myringoplasty. Chi-square tests were used for categorical variables such as gender, smoking status, presence of otorrhoea, ossicular chain status, site of eardrum perforation, type of ossiculoplasty performed, choice of ossiculoplasty material, and postoperative complications, while independent t-tests were employed for continuous variables like age and duration of hearing loss. A p value of < 0.05 was considered statistically significant. | |||
| Group | Patients (N) | preABG | postABG | ΔABG |
|---|---|---|---|---|
| ncCOM | ||||
| CWU mastoidectomy | 61 | 31.4 ± 11.4 dB | 15.8 ± 11.4 dB | 15.5 ± 13.7 dB |
| CWD mastoidectomy | 4 | 40.5 ± 3.7 dB | 16 ± 14.3 dB | 24. ± 13.1 dB |
| p value | 0.119 | 0.980 | 0.213 | |
| cCOM | ||||
| CWU mastoidectomy | 34 | 37.1 ± 13 dB | 16.2 ± 11.9 dB | 20.9 ± 16.7 dB |
| CWD mastoidectomy | 26 | 33 ± 11.6 dB | 13.8 ± 8.5 dB | 19.2 ± 12.3 dB |
| p value | 0.212 | 0.330 | 0.661 | |
| ncCOM | ||||
| PORP | 65 | 29.8 ± 9.8 dB | 15.6 ± 11.2 dB | 14.2 ± 12.6 dB |
| TORP | 8 | 42.2 ± 16.4 dB | 18.3 ± 11.1 dB | 23.8 ± 18.5 dB |
| p value | 0.002 | 0.514 | 0.057 | |
| cCOM | ||||
| PORP | 39 | 30.1 ± 10.2 dB | 14 ± 9.9 dB | 16.1 ± 12.6 dB |
| TORP | 21 | 45.1 ± 10.4 dB | 17.2 ± 11.6 dB | 27.8 ± 15.9 dB |
| p value | < 0.001 | 0.2653 | < 0.001 | |
| Legend: ncCOM: non-cholesteatomatous chronic otitis media; cCOM: cholesteatomatous chronic otitis media; CWU: canal wall up; CWD: canal wall down; PORP: partial ossicular reconstruction prosthesis; TORP: total ossicular reconstruction prosthesis; preABG: preoperative air bone gap; postABG: postoperative air bone gap; ΔABG: difference between pre- and postoperative air bone gap. | ||||
| cCOM | ncCOM | ||||
|---|---|---|---|---|---|
| R2 0.583 | R2 0.376 | ||||
| R2 adjusted 0.569 | R2 adjusted 0.354 | ||||
| ΔABG | Dependent variable | F | p value | F | p value |
| Age | 2.303 | 0.014 | 1.627 | 0.079 | |
| Period of hearing loss | 4.391 | p < 0.001 | 1.436 | 0.147 | |
| Hearing loss type | 0.730 | 0.537 | 0.983 | 0.405 | |
| Otorrhoea | 3.733 | p < 0.001 | 7.616 | p < 0.001 | |
| Site of perforation | 4.063 | p < 0.001 | 1.191 | 0.308 | |
| Ossicular chain status | 2.547 | p < 0.001 | 4.737 | p < 0.001 | |
| Material of OPL | 2.796 | 0.004 | 1.519 | 0.113 | |
| Surgeon | 1.123 | 0.344 | 1.247 | 0.298 | |
| Complications | 38.91 | p < 0.001 | 0.627 | 0.919 | |
| ncCOM: non-cholesteatomatous chronic otitis media; cCOM: cholesteatomatous chronic otitis media; OPL: ossiculoplasty; ΔABG: the difference between pre and postoperative air bone gap. | |||||
References
- Javia L, Ruckenstein M. Ossiculoplasty. Otolaryngol Clin North Am. 2006;39:1177-1189. doi:https://doi.org/10.1016/j.otc.2006.08.010
- Tsetsos N, Vlachtsis K, Stavrakas M. Endoscopic versus microscopic ossiculoplasty in chronic otitis media: a systematic review of the literature. Eur Arch Otorhinolaryngol. 2021;278:917-923.
- Coleman H, Tikka T, Curran J. Comparison of endoscopic vs microscopic ossiculoplasty: a study of 157 consecutive cases. Eur Arch Otorhinolaryngol. 2022;280:89-96. doi:https://doi.org/10.1007/s00405-022-07451-2
- Iannella G, De Vincentiis M, Greco A. Endoscopic approach in second stage ossicular chain reconstruction. Am J Otolaryngol. 2019;40:735-742. doi:https://doi.org/10.1016/j.amjoto.2019.07.004
- Milazzo M, Danti S, Inglese F. Ossicular replacement prostheses from banked bone with ergonomic and functional geometry. J Biomed Mater Res B Appl Biomater. 2017;105:2495-2506. doi:https://doi.org/10.1002/jbm.b.33790
- Sharma M, Pareek Y, Sehra R. Hearing outcome in ossiculoplasty with autologous incus and teflon prosthesis in chronic otitis media: a comparative study. Indian J Otolaryngol Head Neck Surg. 2022;74:345-350. doi:https://doi.org/10.1007/s12070-020-02138-8
- Lamba G, Sohal B, Goyal J. Ossiculoplasty: a prospective study on 50 patients using various graft materials. Indian J Otolaryngol Head Neck Surg. 2019;71:1140-1146. doi:https://doi.org/10.1007/s12070-018-01571-0
- Jung D, Yoo M, Lee K. Comparison of ossiculoplasty outcomes using different materials in the treatment of chronic otitis media. Otol Neurotol. 2021;42:76-81. doi:https://doi.org/10.1097/MAO.0000000000002847
- von Elm E, Altman D, Egger M. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2007;12:1495-1499. doi:https://doi.org/10.1016/j.ijsu.2014.07.013
- Yung M, Tono T, Olszewska E. EAONO/JOS Joint Consensus Statements on the definitions, classification and staging of middle ear cholesteatoma. J Int Adv Otol. 2017;13:1-8. doi:https://doi.org/10.5152/iao.2017.3363
- Yung M, James A, Merkus P. International Otology Outcome Group and the International Consensus on the Categorization of Tympanomastoid Surgery. J Int Adv Otol. 2018;14:216-226. doi:https://doi.org/10.5152/iao.2018.5553
- Dornhoffer J, Gardner E. Prognostic factors in ossiculoplasty: a statistical staging system. Otol Neurotol. 2001;22:299-304. doi:https://doi.org/10.1097/00129492-200105000-00005
- Albu S, Babighian G, Trabalzini F. Prognostic factors in tympanoplasty. Am J Otol. 1998;19:136-140.
- De Vos C, Gersdorff M, Gerard J. Prognostic factors in ossiculoplasty. Otol Neurotol. 2007;28:61-67. doi:https://doi.org/10.1097/01.mao.0000231598.33585.8f
- Sakasi K, Xu A, Ishimoto S. Results of hearing tests after total middle ear reconstruction. Acta Otolaryngol. 2007;127:474-479. doi:https://doi.org/10.1080/00016480600895094
- De Corso E, Barra J, Bernardi F. Role of ossiculoplasty in canal wall down tympanoplasty for middle-ear cholesteatoma: hearing results. J Laryngol Otol. 2007;121:324-328. doi:https://doi.org/10.1017/S0022215106004300
- Sanna M, Shea C, Gamoletti R. Surgery of the “only hearing ear” with chronic ear disease. J Laryngol Otol. 1992;106:793-798. doi:https://doi.org/10.1017/s0022215100120900
- Babighian G. Posterior and attic wall osteoplasty: hearing results and recurrence rates in cholesteatoma. Otol Neurotol. 2002;23:14-17. doi:https://doi.org/10.1097/00129492-200201000-00004
- Redaelli de Zinis L. Titanium vs hydroxyapatite ossiculoplasty in canal wall down mastoidectomy. Arch Otolaryngol Head Neck Surg. 2008;134:1283-1287. doi:https://doi.org/10.1001/archotol.134.12.1283
- Yung N, Brewis C. A comparison of the user-friendliness of hydroxyapatite and titanium ossicular prostheses. J Laryngol Otol. 2002;116:97-102. doi:https://doi.org/10.1258/0022215021910023
- Hajela A, Kumar S, Singh H. Comparison of ossiculoplasty using autograft ossicle versus allograft (teflon). Indian J Otolaryngol Head Neck Surg. 2019;71:1309-1313. doi:https://doi.org/10.1007/s12070-018-1369-5
- Sakai M, Killeen D, Ma C. Audiometric outcomes comparing endoscopic versus microscopic ossiculoplasty. Otol Neurotol. 2022;43:820-826. doi:https://doi.org/10.1097/MAO.0000000000003577
- Potsangbam D, Akoijam B. Endoscopic transcanal autologous cartilage ossiculoplasty. Indian J Otolaryngol Head Neck Surg. 2019;71:54-59. doi:https://doi.org/10.1007/s12070-018-1518-x
- Das A, Mitra S, Ghosh D. Endoscopic ossiculoplasty: is there any edge over the microscopic technique?. Laryngoscope. 2020;130:797-802. doi:https://doi.org/10.1002/lary.28074
- Gülşen S, Çıkrıkcı S. A novel technique in treatment of advanced tympanosclerosis: results of malleus replacement and loop prostheses combination; pure endoscopic transcanal approach. Eur Arch Otorhinolaryngol. 2023;280:3601-3608. doi:https://doi.org/10.1007/s00405-023-07861-w
- Singh K, Nagamani Y, Kour A. A comparative prospective study to evaluate outcomes of ossiculoplasty using autograft versus synthetic graft. Indian J Otolaryngol Head Neck Surg. 2022;74:511-516. doi:https://doi.org/10.1007/s12070-020-02360-4
- Acke F, Kostadinov F, Schlegel C. Reconstructive ossiculoplasty options in primary cholesteatoma surgeries with an intact stapes. Eur Arch Otorhinolaryngol. 2024;281:711-718. doi:https://doi.org/10.1007/s00405-023-08147-x
- Esser J, Klussmann J, Hüttenbrink K. The TORP-PORP: a tympanoplasty technique for isolated defects of the stapes suprastructure. Otol Neurotol. 2024;45:295-298. doi:https://doi.org/10.1097/MAO.0000000000004124
- Lewis A, Backous D, Choi B. Healthcare consumption among subjects with otitis media undergoing middle ear surgery-analysis of cost drivers. Eur Arch Otorhinolaryngol. 2023;280:175-181. doi:https://doi.org/10.1007/s00405-022-07483-8
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2024 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 1354 times
- PDF downloaded - 259 times



