Rhinology
Vol. 44: Issue 5 - October 2024
Utility of intraoperative scoring system in rhino-orbital mucormycosis as a prognostic tool
Abstract
Objective. To assess the utility of an intraoperative scoring system for mucormycosis and to predict prognosis by comparing the score with postoperative outcomes.
Methods. This study was conducted among 80 patients with mucormycosis who underwent surgical management with mandatory pterygopalatine fossa and infratemporal fossa exploration. All cases were scored using our intraoperative scoring assessment tool. Postoperative outcomes in terms of favourable prognosis and mortality were evaluated and compared with demographics, clinical history and intraoperative findings.
Results. An intraoperative score of more than 25 was statistically significant in predicting mortality (p < 0.0001). In all, 86.7% of patients with a score above 25 succumbed to the disease. Statistical significance of mortality (p < 0.05) was observed in those with involvement of pterygopalatine fossa (78.9%), orbit (73.7%), infratemporal fossa (57.9%), cribriform plate (36.8%) and those with history of intake of antiviral drugs (47.4%), use of supplemental oxygen (31.6%) and renal failure (26.3%).
Conclusions. This study enabled better prediction of postoperative prognosis in mucormycosis and reiterated the importance of exploration of pterygopalatine fossa and infratemporal fossa in management and prognostication of invasive fungal sinusitis.
Introduction
Members of the fungal order Mucorales, which includes species like Rhizopus and Mucor, are the source of the fast-progressing infectious illness known as mucormycosis 1. It is an acute, aggressive, and opportunistic illness that is more common in immunocompromised people and has been linked to a high fatality rate. Based on the site of involvement, it can be characterised as rhinocerebral, pulmonary, gastrointestinal, or disseminated. The mortality rate of this disease has been as high as 40% for many decades despite aggressive therapy 2.
The pterygopalatine fossa (PPF) is a tiny fat-filled area in the skull that can act as an inconspicuous space for the proliferation of mucor. The PPF serves as a relay station for many neurovascular structures, making it a crucial channel that helps an infection to quickly spread to neighbouring essential structures, including the retro-global space of the orbit and the infratemporal fossa (ITF) 2. The orbit is often reachable via the ethmoid bone’s lamina papyracea, ITF, inferior orbital fissure, or orbital apex, while the cribriform plate, supraorbital fissure, and perineural invasion are usual entryways for intracranial extension 2. Therefore, the spread of infection into the PPF and ITF necessitates immediate surgical debridement as well as vigorous antifungal treatment.
Mucormycosis is the third most frequent invasive fungal infection in the world, behind invasive candidal mycosis and invasive aspergillosis, and has caused the most morbidity and mortality worldwide 3. In the second wave of the SARS-CoV-2 pandemic (COVID-19), a startling and unexpected surge in mucormycosis cases was seen among patients who tested positive for COVID-19, particularly rhino-orbital-cerebral mucormycosis (ROCM) 4,5. Although there were just a few mucormycosis cases in the initial stages of the pandemic, the enormous increase that reached epidemic proportions led to the term COVID-Associated Mucormycosis (CAM) being coined 6. Even prior to the pandemic, India contributed to the highest disease burden 7 and had a higher prevalence than many affluent nations (about 0.14 cases per 1000 individuals) 8.
During the initial course of the disease, mucormycosis often presents similar to sinusitis or orbital cellulitis. Because the symptoms are nonspecific and might resemble a less serious infection, the patient’s clinical presentation, as well as the diagnostic work-up and care, are frequently delayed 9. Before the second wave of the COVID-19 pandemic, most mucor occurrences were sporadic, with patients presenting late in the course of their illness 6. Although radiological imaging offers a fair image of the disease’s extent, it may not be as informative early in the course of the disease as it only reveals abnormalities, such as inflammation of the paranasal sinuses 10. As a result, PPF involvement may not be obvious, and it may only be visualised while operating on the patient after the seemingly normal posterolateral wall of the maxilla and pterygoid plates have been removed 5. Exploration of the PPF is thus a critical step in determining the extent and hidden focus of infection, and failure to do so may result in poor postoperative prognosis and recurrence of infection even in a patient with normal clinical or radiological findings 2.
Despite the unexpected spike in CAM cases and accompanying morbidity and mortality in the last few years, there is a dearth of good tools and systems for the staging and prognosis of this illness. During the initial months of the COVID-19 pandemic, a pilot study was conducted over 3 months on patients suffering from CAM, and an intraoperative scoring system was introduced by Shenoy et al. (Tab. I) 2. From January 2021 to March 2022, 80 cases of mucormycosis, both CAM and non-CAM, have been operated in our institution. The current study aims to assess the utility of this scoring tool based on intraoperative observations for prognosticating mucormycosis and determining the need for surgical clearance of various subsites. Through this study, we also aim to examine and compare the prognosis in terms of postoperative outcome with the clinical history, c-reactive protein (CRP) levels, and intraoperative scores.
Materials and methods
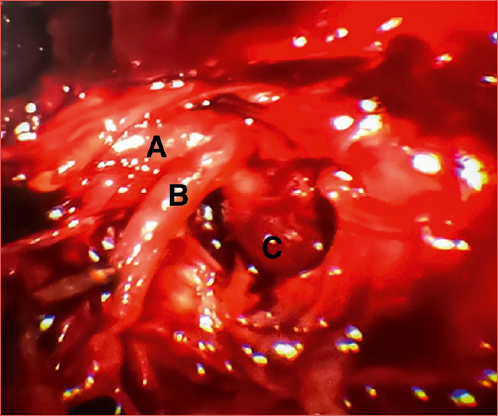
The retrospective observational study was carried out in a tertiary referral centre in Southern India. All patients proven to have mucormycosis based on a KOH mount or fungal culture and sensitivity were included in the study, while patients without nasal involvement or those who underwent surgery elsewhere were excluded. All subjects underwent imaging by both 1.5 Tesla magnetic resonance imaging (MRI) with gadolinium contrast and 36-slice computed tomography (CT). The patients underwent surgical debridement, i.e., Denker’s procedure – endoscopic sinus surgery with mandatory PPF and ITF exploration in all, irrespective of radiological involvement (Cover figure). A total maxillectomy was preferred for patients with significant disease in whom endoscopic clearance was not achievable, whereas those with orbital involvement additionally underwent endoscopic orbital debridement.
All cases were given a score based on intraoperative findings, using a scoring assessment tool for mucormycosis designed by Shenoy et al. (Tab. I) 2. The highest possible score is 45. Individual points were assigned to different components based on their degree of involvement intraoperatively and later confirmed histopathologically. Bilaterally, each of the sinuses was given scores ranging from 0-2. The septum, middle turbinate, inferior turbinate, and floor of the nasal fossa were also each given scores of 0-2. Depending on the degree of involvement, the cribriform plate and orbit were scored up to 3 points and 2 points, respectively. The involvement of fat, vessels, nerves, and muscles in the PPF and ITF was noted, and each component was scored between 0 and 2. The scores assigned to each subsite were then added. In the postoperative period, none of the patients in our series developed any surgical complications. All patients received injections of liposomal amphotericin B (5-10 mg/kg) and subsequently oral posaconazole (600 mg on day 1 and then 300 mg per day from day 2). Renal function tests and CRP were performed on an alternate-day basis during therapy to assess treatment response and monitor for adverse effects.
After obtaining approval from the Institutional Ethics Committee, data was collected. The clinical history, radiological investigation findings, intraoperative notes, and course of treatment were studied for each patient. The findings were documented, and appropriate statistical tools were applied to compare the prognosis of the disease with the clinical history, CRP levels, and intraoperative scores. The prognosis was evaluated by measuring mucormycosis-associated mortality postoperatively at the end of two months of completed treatment. An independent sample t-test was performed to compare the mean age, mean CRP, and mean intraoperative score between those who succumbed to the disease and those who recovered. Fisher’s Exact test was used to determine the association between the two groups and categorical variables such as sex, history of pre-existing diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD), renal failure (RF), history of prior hospitalisation, history of intake of corticosteroids, supplemental oxygen, anti-viral medication, and zinc (Zn) supplements. The same test was also applied to evaluate the association between the involvement of the nasal cavity, paranasal sinuses, ITF, PPF, orbit, and cribriform plate with postoperative outcomes.
Results
Patient demographics
Eighty individuals were included in the study: 19 females and 61 males. The average age of patients at the time of their hospital visit was 50 years (range: 25-77). The mean age of patients who recovered from the disease was 49 years, whereas the average age of those who succumbed to the disease was 54 years.
Clinical history
Around 21% of patients had pre-existing diabetes, 12.5% had COPD, and 10% had RF. A history of hospitalisation was seen in 10% of subjects. Corticosteroid and antiviral drug use were reported by 20% and 15% of patients, respectively; 12.5% of patients reported using supplemental oxygen in the past, whereas 11.2% of individuals had previously taken zinc supplements. The analysis between the clinical history and prognosis was statistically significant for the history of antiviral drug intake (p < 0.0001), use of Zn supplements (p = 0.0004), use of supplemental oxygen (p = 0.0098) and RF (p = 0.0163), but not for a history of pre-existing DM, COPD, hospitalisation or use of corticosteroids (Tab. II).
Biochemical investigations
While the average CRP level in all patients was 142, the mean preoperative CRP levels in those who survived and in those who passed away from the illness were 133 and 179 mg/L, respectively.
Involvement of various subsites, as visualised intraoperatively
In this study, sinus involvement and nasal cavity involvement were observed intraoperatively in all patients. Intraoperatively, involvement of the PPF and ITF was observed in 47.5% and 21.2% of patients, respectively, while the orbit and cribriform plate were involved in 36.2% and 12.5% of patients, respectively. Close to 80% of people who did not survive the disease had PPF involvement (Fig. 1). More than 85% of those who survived did not have ITF involvement (Fig. 2). Ninety-five percent of patients who did not have orbital involvement survived (Fig. 3). It was observed that more than 95% of survivors lacked cribriform plate involvement, whereas 70% of those who did, did not survive the disease (Fig. 4). Statistical significance was seen between mortality in mucormycosis and intraoperative involvement of the orbit (p = 0.0002), ITF (p = 0.0004), cribriform plate (p = 0.0012) and PPF (p = 0.0031) (Tab. III).
Novel intraoperative scoring tool
In this study, mucormycosis-associated postoperative mortality and intraoperative scores were compared. We decided to set the cut-off score in this novel research at 25 out of 45 since the statistical analysis for calculating the cut-off could not be evaluated due to the limited sample size. The lowest score observed in our study was 10, while the highest was 38. The lowest documented score of individuals who succumbed to the condition was 15, while the highest was 38. The mean score of those who survived was 17.5, while it was 27.1 for those who succumbed to mucormycosis. Most patients who survived had an intraoperative score of less than or equal to 25. At the end of two months, 19 subjects succumbed to the disease, of which 13 had scores of more than 25. A total of 23.7% succumbed to the disease, and all had a score of ≥ 15, while 18.7% of patients had an intraoperative score of more than 25, and more than 86% succumbed to the disease. Among the 19 patients who passed away from the illness, 15 patients had undergone endoscopic Denker’s approach with PPF and ITF clearance, while the remaining underwent total maxillectomy. At the end of 2 months 33.3% of females and 20.9% of males did not survive the illness. Postoperatively, cases with intraoperative scores greater than 25 were observed to have higher mortality (p < 0.0001) (Fig. 5).
Discussion
Mucormycosis is an angio-invasive disease characterised by the haematogenous dissemination of infection. ROCM spreads in a distinct manner. Inhaled fungus spores germinate into hyphae in the sinuses, where they then move to the orbit and cranium through blood vessels and neuronal connections, and via the foramina into the maxilla 11. Rather than by bony erosion, the infection advances to the majority of surrounding tissues, including the ITF and orbit, via neurovascular pathways 5.
Although the aetiology of mucormycosis is unclear, some theories suggest that prolonged and inappropriate administration of corticosteroids 12, peripheral microthrombi 11, COVID-19-induced immune dysregulation and immunosuppression, and uncontrolled DM are causative factors of mucormycosis because they favour the growth of Mucorales 4,13. Immunocompromised individuals, such as those who have undergone transplants or who have neutropenia or malignancy, are at an elevated risk of getting mucormycosis 4. Additionally, people receiving chemotherapy and those with hepatic or renal insufficiency both exhibit a higher risk of infection 5. Unsupervised use of antibiotics and the use of zinc and vitamin C tablets in large quantities for extended lengths of time in the middle of the health calamity with inadequate healthcare facilities in resource-constrained nations like India could have contributed to the rise in CAM cases 13. All these factors, particularly the indiscriminate use of steroids, might have contributed to the abrupt spike in ROCM cases during the COVID-19 pandemic’s second wave 14. The increased number of mucormycosis cases during the pandemic provided us with an opportunity to study the illness and evaluate the utility of an intraoperative scoring tool (Tab. I).
Mucormycosis can be classified as a sinonasal disease, rhino-orbital disease, or ROCM, based on the extent of the disease 2. The paranasal sinuses are initially impacted by ROCM, after which there is an eventual extension into the orbit and cranium 9. Most patients present with nose block, headache, facial pain and numbness, periorbital oedema, and visual complaints ranging from mild to severe ophthalmoplegia 4. Additionally, they may present with a blackish necrotic lesion over the hard palate, nasal mucosa, skin, or orbit 2. They may also exhibit signs as severe as cavernous sinus thrombosis as well as intracranial dissemination, such as cranial nerve palsies 6.
To accurately diagnose the disease and its extent, especially in the initial stages when radiological results are non-specific, a thorough history and physical examination that includes the examination of the oral cavity, nose, eyes, and cranial nerves is of paramount importance. A study by Slonimsky et al. revealed that while bone erosions are a specific sign of invasive fungal infections, they are also very insensitive signs, and patients with bony invasion did not necessarily exhibit erosions on CT scans 15. In a study by Hada et al., lamina papyracea breach was noted on MRI in 26.9% of patients, although it was intraoperatively seen in 37.2% of patients, and the sensitivity of MRI in detecting medial orbital wall defect and erosion of lamina papyracea is only about 65% 16. Similarly, in 23 of 43 cases, involvement of the PPF and ITF was not detected on imaging, but only became apparent during surgical exploration 2. In the literature, involvement of various subsites by mucor was underestimated with imaging modalities. Hence, we performed mandatory exploration of compartments for better disease clearance. This surgical approach is outside current guidelines and larger studies are needed to demonstrate its efficacy and safety.
Even in the absence of damage to the bony wall of the sinuses, inflammation around the sinuses should prompt us to strongly consider severe disease with potential spread to the PPF, ITF, orbit, or cavernous sinus 17. In our study, we found that it is important to intraoperatively score the involvement of these subsites, as it gives us a better understanding of the severity of the disease. It is also imperative to intraoperatively visualise them, especially the PPF, as it also gives an idea of the spread of mucormycosis and the severity of disease (Cover figure). Intraoperative complications such as bleeding, CSF leak, orbital haematoma, nasolacrimal duct trauma and periorbital oedema have been noted in the literature 18. However, such complications were not encountered in our series, presumably due to the meticulous surgical dissection taken in order to do the scoring as per the tool (Tab. IV).
The PPF, being one of the main reservoirs for mucor, contributes to the disease’s rapid spread. Regardless of the evidence of clinical or radiological involvement and the technique or extent of the operation, the posterior wall of the maxillary sinus should be removed. This step is critical in achieving full disease clearance and lowering the risk of postoperative recurrence and mortality.
Numerous studies have been done on mucormycosis, but most have focused on the epidemiology, clinical picture, and imaging. There is no reliable staging system in place to prognosticate mucormycosis. One of the few scoring systems developed is by Shah et al., which considers clinical presentation, radiological, and ophthalmological findings, with a cut-off score of 23 that establishes the stage at which orbital exenteration is imperative 21. Ulas et al. used the same scoring system and found that a score of 18 was the threshold 22. Honavar 23 and Naik et al. 24 have also proposed staging systems for ROCM in the COVID setting that are based on nasal, paranasal, orbital, and cerebral signs and radiological imaging of these subsites. Shenoy et al. thoroughly examined and scored numerous subsites of mucormycosis while operating on CAM patients to establish an intraoperative evaluation scoring system with a cut-off score of 25 2. Each subsite was scored to help the surgeon understand the severity of the illness and to prognosticate the disease outcome after treatment. To the best of our knowledge, this scoring system is a unique and innovative intraoperative scoring system for mucormycosis. Unlike other studies, it also takes the intraoperative involvement of PPF and ITF into account, thus giving a more accurate representation of the disease burden and a better understanding on the need for surgical clearance. In our study, the postoperative prognosis of the patients was determined using this scoring method. An intraoperative score of more than 25 was seen in 18.7% of patients. Out of the patients who succumbed to the disease, more than 68% were found to have scores more than 25, while all patients had a score of more than or equal to 15.
A regression analysis by Moorthy et al. 6 revealed that the age of the patient, glycaemic control, and intra-orbital involvement were significant predictors of survival. According to their research, the log of the odds of survival decreased with each unit increase in age and HbA1c by 0.043 and 0.328, respectively, although the absence of intra-orbital involvement increased the log of the odds of survival by 1.176 6. In our investigation, subjects with scores greater than 25 had a higher postoperative death rate (68.4%). The factors that correlated with mortality were involvement of the PPF, orbit, ITF, and cribriform plate, and patients with a history of pre-existing renal failure, use of supplemental oxygen and intake of antiviral drugs and Zn supplements. Due to the extensive scoring of each subsite in this study, this intraoperative scoring system gives more precise insights into the severity of mucormycosis.
Since mucormycosis is a rare illness, the number of patients reporting to the hospital is low. To analyse the involvement of various subsites and the necessity for surgical clearance, we excluded patients with mucormycosis who had already been operated on, resulting in a smaller cohort. Due to this, a regression analysis could not be performed to quantify the influence of various comorbidities and subsite participation. Furthermore, a cut-off value for the intraoperative score could not be statistically derived owing to the limited sample size. The value was determined by the authors based on their experience and clinical acumen.
The novel intraoperative scoring system used in this study is helpful in improving the prediction of postoperative outcomes in mucormycosis. Although the use of this tool is limited by the lack of validation, we think it can be used by clinicians handling future cases to predict the prognosis in patients with mucormycosis and other invasive fungal sinusitis. We propose global collaboration to validate this intraoperative prognostic tool, which is conducive to superior postoperative prognosis.
Conclusions
This study has reiterated the importance of the exploration of PPF and ITF in the prognostication of mucormycosis. It has also been demonstrated that a thorough clinical history can help identify risk factors that may hint at poorer prognosis. Although this study was conducted on patients with mucormycosis, we believe that the results may be extended to all invasive fungal mycoses.
Acknowledgements
The authors acknowledge all the colleagues of Otorhinolaryngology Head and Neck Surgery Unit of Kasturba Medical College and Hospital, MAHE for their contribution to this study.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
NZ, VSS, SB, SKK: contributed significantly to the conception and design of the work; NZ, VSS: contributed significantly to drafting the work. All the authors made a major contribution to data collection, analysis, and interpretation. All authors have finally approved the version to be published and agree to be accountable and responsible for all aspects of the work to ensure that questions or problems concerning the accuracy, integrity, quality, or credibility of any part of the work are adequately investigated, reviewed, and resolved.
Ethical consideration
This study was approved by the Institutional Ethics Committee, Kasturba Medical College, Mangalore (IEC KMC MLR 08/2022/378). The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
Written informed consent was obtained from each participant/patient for study participation and data publication.
History
Received: July 29, 2023
Accepted: June 13, 2024
Figures and tables
Figure 1. Comparison of involvement of PPF with mortality in mucormycosis.
Figure 2. Comparison of involvement of ITF with mortality in mucormycosis.
Figure 3. Comparison of involvement of orbit with mortality in mucormycosis.
Figure 4. Comparison of involvement of cribriform plate with mortality in mucormycosis.
Figure 5. Comparison of the intraoperative score with mortality in mucormycosis.
| Sinus involvement | Right sinus | Left sinus |
|---|---|---|
| Maxillary | 0-2 | 0-2 |
| Ethmoid | 0-2 | 0-2 |
| Sphenoid | 0-2 | 0-2 |
| Frontal | 0-2 | 0-2 |
| (0 – no involvement; 1 – mucosal involvement; 2 – bone involvement) | ||
| Nasal cavity | ||
| Septum | 0-2 | |
| Middle turbinate | 0-2 | |
| Inferior Turbinate | 0-2 | |
| Floor | 0-2 | |
| (0 – no involvement; 1 – mucosal involvement; 2 – bone involvement) | ||
| Cribriform plate | 0-3 | |
| (0 – no involvement; 1 – mucosal involvement; 2 – bone involvement; 3 – intracranial extension) | ||
| Orbital involvement | 0-2 | |
| (0 – no involvement; 1 – lamina papyracea extraconal involvement; 2 – intraconal involvement) | ||
| Pterygopalatine fossa involvement | ||
| Fat | 0-2 | |
| (0 – no involvement; 1 – inflamed; 2 – necrosed) | ||
| Vascular compartment | 0-2 | |
| (0 – no involvement; 1 – involvement seen; 2 – thrombosed/necrosed) | ||
| Neural compartment | 0-2 | |
| (0 – no involvement; 1 – inflamed; 2 – necrosed) | ||
| Muscular compartment | 0-2 | |
| (0 – no involvement; 1 – inflamed; 2 – necrosed) | ||
| Infratemporal fossa involvement | ||
| Fat | 0-2 | |
| (0 – no involvement; 1 – inflamed; 2 – necrosed) | ||
| Vascular compartment | 0-2 | |
| (0 – no involvement; 1 – involvement seen; 2 – thrombosed/necrosed) | ||
| Neural compartment | 0-2 | |
| (0 – no involvement; 1 – inflamed; 2 – necrosed) | ||
| Muscular compartment | 0-2 | |
| (0 – no involvement; 1 – inflamed; 2 – necrosed) | ||
| Variables | Mortality | p value | |
|---|---|---|---|
| Alive (N = 61) | Dead (N = 19) | ||
| Age | 0.7267 | ||
| Mean ± SD | 48.7 ± 11.8 | 54.3 ± 10.9 | |
| Min - Max | 25-77 | 33-77 | |
| CRP (mg/L) | |||
| Mean ± SD | 132.7 ± 66.8 | 169.6 ± 67.5 | |
| Min - Max | 30-268 | 64-295 | |
| Intraoperative Score | 0.2876 | ||
| Mean ± SD | 17.5 ± 5.1 | 27.1 ± 6.2 | |
| Median | 16 | 28 | |
| Q1-Q3 | 14-20 | 22-31 | |
| Min - Max | 10-38 | 15-38 | |
| Intraoperative Score ≤ 25 | 59 (96.7%) | 6 (31.5%) | < 0.0001* |
| Intraoperative Score > 25 | 2 (3.2%) | 13 (68.4%) | |
| Sex | 0.3470 | ||
| Male | 49 (80.3%) | 13 (68.4%) | |
| Female | 12 (19.6%) | 6 (31.5%) | |
| Pre-existing DM | 1.0000 | ||
| No | 48 (78.6%) | 15 (78.9%) | |
| Yes | 13 (21.3%) | 4 (21%) | |
| Pre-existing COPD | 0.2373 | ||
| No | 55 (90.1%) | 15 (78.9%) | |
| Yes | 6 (9.8%) | 4 (21%) | |
| Pre-existing RF | 0.0163* | ||
| No | 58 (95%) | 14 (73.6%) | |
| Yes | 3 (4.9%) | 5 (26.3%) | |
| History of prior hospitalisation | 0.3865 | ||
| No | 56 (91.8%) | 16 (84.2%) | |
| Yes | 5 (8.2%) | 3 (15.7%) | |
| History of corticosteroid use | 0.5135 | ||
| No | 50 (81.9%) | 14 (73.6%) | |
| Yes | 11 (18%) | 5 (26.3%) | |
| History of antiviral use | < 0.0001* | ||
| No | 58 (95%) | 10 (52.6%) | |
| Yes | 3 (4.9%) | 9 (47.3%) | |
| History of use of supplemental O 2 | 0.0098* | ||
| No | 57 (93.4%) | 13 (68.4%) | |
| Yes | 4 (6.5%) | 6 (31.5%) | |
| History of Zn supplement intake | 0.0004* | ||
| No | 59 (96.7%) | 12 (63.1%) | |
| Yes | 2 (3.2%) | 7 (36.8%) | |
| p value is derived from Fisher’s Exact test. | |||
| * p value is statistically significant. | |||
| Variables | Mortality | p value | |
|---|---|---|---|
| Alive (N = 61) | Dead (N = 19) | ||
| Sinus involvement | NA | ||
| Absent | 0 | 0 | |
| Present | 61 (100%) | 19 (100%) | |
| Nasal cavity | NA | ||
| Absent | 0 | 0 | |
| Present | 61 (100%) | 19 (100%) | |
| Cribriform plate | 0.0012* | ||
| Absent | 58 (95%) | 12 (63.1%) | |
| Present | 3 (4.9%) | 7 (36.8%) | |
| Orbit involvement | 0.0002* | ||
| Absent | 46 (75.4%) | 5 (26.3%) | |
| Present | 15 (24.5%) | 14 (73.6%) | |
| Pterygopalatine involvement | 0.0031* | ||
| Absent | 38 (62.3%) | 4 (21%) | |
| Present | 23 (37.7%) | 15 (78.9%) | |
| Infratemporal involvement | 0.0004* | ||
| Absent | 52 (85.2%) | 11 (57.8%) | |
| Present | 9 (14.7%) | 8 (42.1%) | |
| p value is derived from Fisher’s Exact test. | |||
| * p value is statistically significant. | |||
| Study | Mittal et al. 19 | Jindal et al. 20 | Our study |
|---|---|---|---|
| Seen | Radiologically | Radiologically | Intraoperatively |
| PPF | 90% | 47% | 47.5% |
| ITF | - | 60% | 21.1% |
| Orbit | 78% | - | 36.2% |
| Intracranial | 44% | 60% | 12.5% |
References
- Skiada A, Pavleas I, Drogari-Apiranthitou M. Epidemiology and diagnosis of mucormycosis: an update. J Fungi. 2020;6:1-20. doi:https://doi.org/10.3390/jof6040265
- Shenoy V, Bajpai S, Kasargod S. Intraoperative scoring assessment as a prognostic tool in COVID-19 associated mucormycosis: a short-term observational study. Indian J Otolaryngol Head Neck Surg. 74:3521-3525. doi:https://doi.org/10.1007/s12070-021-03015-8
- Koehler P, Mellinghoff S, Lagrou K. Development and validation of the European QUALity (EQUAL) score for mucormycosis management in haematology. J Antimicrob Chemother. 2019;74:1704-1712. doi:https://doi.org/10.1093/jac/dkz051
- Mitra S, Janweja M, Sengupta A. Post-COVID-19 rhino-orbito-cerebral mucormycosis: a new addition to challenges in pandemic control. Eur Arch Otorhinolaryngol. 2022;279:2417-2422. doi:https://doi.org/10.1007/s00405-021-07010-1
- Pal P, Singh B, Singla S. Mucormycosis in COVID-19 pandemic and its neurovascular spread. Eur Arch Otorhinolaryngol. 2022;279:2965-2972. doi:https://doi.org/10.1007/s00405-021-07106-8
- Moorthy A, Nayak T, Bachalli P. COVID-associated rhinocerebral mucormycosis: a retrospective analysis of presentation and outcomes. Eur Arch Otorhinolaryngol. 2023;280:713-721. doi:https://doi.org/10.1007/s00405-022-07544-y
- Joshi S, Telang R, Tambe M. Outbreak of mucormycosis in coronavirus disease patients, Pune, India. Emerg Infect Dis. 2022;28:1-8. doi:https://doi.org/10.3201/eid2801.211636
- Chander J, Singla N, Kaur M. Saksenaea erythrospora, an emerging mucoralean fungus causing severe necrotizing skin and soft tissue infections – a study from a tertiary care hospital in north India. Infect Dis (Lond). 2017;49:170-177. doi:https://doi.org/10.1080/23744235.2016.1239027
- Beiglboeck F, Theofilou N, Fuchs M. Managing mucormycosis in diabetic patients: a case report with critical review of the literature. Oral Dis. 2022;28:568-576. doi:https://doi.org/10.1111/odi.13802
- Narayanan S, Panarkandy G, Subramaniam G. The “black evil” affecting patients with diabetes: a case of rhino orbito cerebral mucormycosis causing Garcin syndrome. Infect Drug Resist. 2017;10:103-108. doi:https://doi.org/10.2147/IDR.S130926
- Moorthy A, Gaikwad R, Krishna S. SARS-CoV-2, uncontrolled diabetes and corticosteroids – An Unholy trinity in invasive fungal infections of the maxillofacial region? A retrospective, multi-centric analysis. J Maxillofac Oral Surg. 2021;20:418-425. doi:https://doi.org/10.1007/s12663-021-01532-1
- Ahmadikia K, Hashemi S, Khodavaisy S. The double-edged sword of systemic corticosteroid therapy in viral pneumonia: a case report and comparative review of influenza-associated mucormycosis versus COVID-19 associated mucormycosis. Mycoses. 2021;64:798-808. doi:https://doi.org/10.1111/myc.13256
- Radotra B, Challa S. Pathogenesis and pathology of COVID-associated mucormycosis: what is new and why. Curr Fungal Infect Rep. 2022;16:206-220. doi:https://doi.org/10.1007/s12281-022-00443-z
- Ravindra K, Ahlawat A. Five probable factors responsible for the COVID-associated mucormycosis outbreak in India. Int J Infect Dis. 2021;112:278-280. doi:https://doi.org/10.1016/j.ijid.2021.09.057
- Slonimsky G, Slonimsky E, Yakirevitch A. The significance of Computed Tomography in invasive paranasal mucormycosis. Rhinology. 2018;56:54-58. doi:https://doi.org/10.4193/Rhin17.153
- Hada M, Gupta P, Bagarhatta M. Orbital magnetic resonance imaging profile and clinicoradiological correlation in COVID-19-associated rhino-orbital-cerebral mucormycosis: a single-center study of 270 patients from North India. Indian J Ophthalmol. 2022;70:641-648. doi:https://doi.org/10.4103/ijo.IJO_1652_21
- Raab P, Sedlacek L, Buchholz S. Imaging patterns of rhino-orbital-cerebral mucormycosis in immunocompromised patients: when to suspect complicated mucormycosis. Clin Neuroradiol. 2017;27:469-475. doi:https://doi.org/10.1007/s00062-017-0629-1
- Chaurpagar R, Chiplunkar B, Doifode P. Study of clinicoepidemiology and surgical complications in acute invasive fungal rhinosinusitis. Indian J Otolaryngol Head Neck Surg. 2023;75:867-874. doi:https://doi.org/10.1007/s12070-022-03430-5
- Mittal A, Mahajan N, Pal Singh DD. SARS-CoV-19-associated rhino-orbital and cerebral mucormycosis: clinical and radiological presentations. Med Mycol. Published online 2022. doi:https://doi.org/10.1093/MMY/MYAC045
- Jindal G, Sethi A, Bhargarva K. Imaging findings in invasive rhino-orbito-cerebral mucormycosis in post-COVID-19 patients. Proc (Bayl Univ Med Cent). 2021;35:32-34. doi:https://doi.org/10.1080/08998280.2021.1981100
- Shah K, Dave V, Bradoo R. Orbital exenteration in rhino-orbito-cerebral mucormycosis: a prospective analytical study with scoring system. Indian J Otolaryngol Head Neck Surg. 2019;71:259-265. doi:https://doi.org/10.1007/s12070-018-1293-8
- Ulas B, Kursun E, Turunc T. Scoring system evaluation for orbital exenteration in patients with rhino-orbito-cerebral mucormycosis. J Fr Ophtalmol. 2022;45:47-52. doi:https://doi.org/10.1016/j.jfo.2021.07.008
- Honavar S. Code mucor: guidelines for the diagnosis, staging and management of rhino-orbito-cerebral mucormycosis in the setting of COVID-19. Indian J Ophthalmol. 2021;69:1361-1365. doi:https://doi.org/10.4103/ijo.IJO_1165_21
- Naik M, Rath S. The ROC staging system for COVID-related rhino-orbital-cerebral mucormycosis. Semin Ophthalmol. 2022;37:279-283. doi:https://doi.org/10.1080/08820538.2021.1946094
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2024 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 323 times
- PDF downloaded - 97 times




 PDF
PDF
