Head and neck
Vol. 44: Issue 5 - October 2024
Modular anatomic approach to oral tongue carcinoma: functional outcomes and quality of life
Abstract
Objectives. The purpose of this study is to present the long-term functional swallowing outcomes of various surgical approaches to oral tongue/floor of mouth squamous cell carcinoma (OTFOMSCC) according to a modular and compartment-based concept previously described elsewhere.
Methods. A retrospective study was conducted on patients undergoing surgery for OTFOMSCC from January 2017 to April 2023 in the Department of Otorhinolaryngology at the Hospital of Bolzano. Functional swallowing outcomes and quality of life (QoL) were assessed through the administration of a scale and questionnaires between 6 months and 1 year postoperatively or after the end of adjuvant therapy, stratifying the results according to the surgical technique used.
Results. A total of 92 patients with OTFOMSCC were enrolled: 44 patients underwent transoral anatomically guided surgery (TAGS) for early-stage tumours, and 48 underwent major surgery for advanced stages. Among the latter 48 patients: 35 underwent compartment tongue surgery (CTS), 3 underwent extended glossectomies (EG) Type A, 6 underwent EG Type B, and 4 underwent EG Type C. After TAGS, all patients resumed oral feeding for all consistencies. In the CTS group, only one patient faced challenges with pure liquids, yet all achieved the target of consuming a semisolid and semiliquid diet. EG exhibited a noticeable decline in performance from Type A to total glossectomy (Type C).
Conclusions. Following an anatomically-guided approach to the resection of OTFOMSCC allows the surgery to be modulated on the structures involved by the tumour, thus achieving optimal oncological results, while maintaining the possibility to predict functional outcomes and postoperative QoL.
Introduction
Malignant tumours of the oral cavity are the most common neoplasms in the head and neck region 1,2. The most frequent site is represented by the mobile tongue 3. The most widespread histology is squamous. Currently, the gold standard therapeutic approach for oral tongue/floor of mouth squamous cell carcinoma (OTFOMSCC) is surgery. The standard of care involves the removal of the primary lesion with surrounding macroscopic margins of approximately 0.5-2 cm. Compartmental tongue surgery (CTS), proposed by Calabrese et al. in 2009 4, is a surgical technique whose aim is to remove the entire oncological compartment simultaneously with potential pathways of tumour spread. These include the affected part of the tongue, the cervical lymph nodes, and the so-called “tumour-nodes tract” (TNT) 4-7. The goal is the complete removal of the tumour within the compartment, which may potentially harbour perineural and/or lymphovascular disease progression, as well as micrometastases in transit or satellite tumours, thus ensuring improved local and locoregional control 7.
The anatomically-guided approach to tongue neoplasms, following the principles of compartmental surgery, can be tailored based on the tumour’s depth and the involved musculature. Depending on the tumour’s characteristics, various surgical approaches can be proposed, ranging from transoral surgery to CTS, potentially extended to the contralateral hemitongue. CTS has shown excellent oncological outcomes in terms of both disease-specific survival (DSS) and overall survival (OS). One of the main criticisms against this type of surgical approach concerns its apparent aggressiveness and the theoretically unfavourable implications for functionality. As theorised by Calabrese and colleagues 8, once muscle fibres are severed, they are no longer functional and can create scar tissue that envelops the residual portion of the tongue, reducing its range of motion. For this reason, the reconstruction of this defect using a free or pedicled flap, depending on the patient’s characteristics, is mandatory to separate the oral cavity from the neck and maintain the unaffected hemitongue capable of movement and of compensating for the absence of the contralateral compartment 9,10.
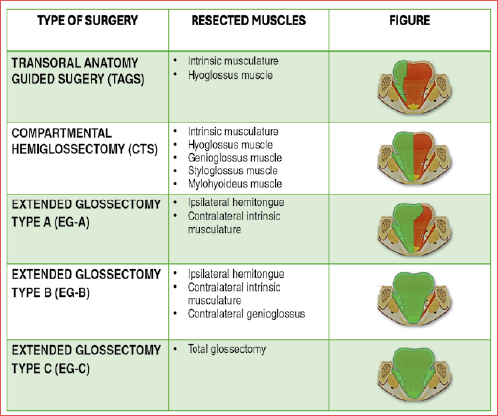
The purpose of this study is to present the long-term functional swallowing outcomes of various surgical approaches to OTFOMSCC according to a modular and compartment-based concept described by Calabrese et al. 4,7,11,12: transoral surgery including the TNT tract (transoral anatomically guided surgery, TAGS), unilateral CTS, and extended glossectomies (EG) beyond the ipsilateral hemitongue (Cover figure). Swallowing outcomes are analysed based on both objective and subjective assessments, stratifying the results according to the surgical technique used.
Materials and methods
A retrospective study was conducted on patients who underwent surgery for OTFOMSCC between January 2017 and April 2023 in the Department of Otorhinolaryngology-Head and Neck Surgery at the Central Hospital of Bolzano.
Inclusion criteria were:
- Patients affected by OTFOMSCC cT1-cT4 extending to adjacent subsites;
- Those undergoing TAGS, CTS, and EG Type A, Type B, and Type C;
- Patients of 18 years of age or older;
- Patients with a functional swallowing follow-up between 6 months and 1 year after surgery or end of adjuvant therapy;
- Patients who provided informed consent to participate in the study.
Exclusion criteria were:
- Patients not functionally assessed in terms of swallowing during follow-up;
- Patients with less than 6 months of follow-up;
- Unavailable data.
Preoperative management
In patients with cT3-4 OTFOMSCC and all cT2 cases with suspected deep infiltration, the preferred imaging technique was contrast-enhanced MRI, aiming to assess tumour extension, potential infiltration of soft tissues and possible involvement of the mandible. In cases where MRI was contraindicated due to the presence of vascular clips, prosthetic implants, or claustrophobia, patients underwent contrast-enhanced CT. Ultrasound was routinely used to assess lymph node status, with ultrasound-guided needle aspiration in cases of suspected lymph node metastasis.
For patients with advanced-stage OTFOMSCC, a PET-CT or total-body CT was performed before surgery to evaluate the presence of distant metastases. Staging of patients was conducted according to the 8th Edition of the TNM Staging System 13.
Patients with early-stage OTFOMSCC (cT1-2) without lymph node metastasis (cN0) and with clinically and radiologically confirmed absence of infiltration of the extrinsic musculature underwent TAGS, with delayed lymph node dissection based on the pathological stage of the disease. The TAGS technique followed the surgical steps previously described 11,14. Candidates for TAGS are those with early-stage cT1-T2 N0 tumours. At our centre, the first procedure performed is transoral excision of the primary tumour. Based on the histological examination, elective neck dissection is indicated if the pathological DOI is greater than 4 mm or if there are adverse factors such as lymphovascular invasion or high-grade lesion. Elective neck dissection is performed within one month from transoral surgery. The advantage is two fold: firstly, a more precise indication for dissection based on histopathological parameters, and secondly, it allows for the healing of the primary intraoral tumour site, avoiding the risk of fistulas.
Patients with advanced-stage OTFOMSCC underwent unilateral CTS or EG Type A, B, or C based on the local extension of the disease and ipsilateral, bilateral, or contralateral lymph node dissection (depending on lymph node status, previous treatments, and the site of the primary tumour). Concurrent reconstruction of the surgical defect was performed using a free or pedicled flap, depending on the surgical defect and the patient’s overall condition.
Regarding CTS and EG Type A, B, and C, the surgical steps previously described were followed 7,12. The Cover figure shows the classification of the different types of glossectomies.
All patients scheduled for major oral cavity surgery (CTS or EG) underwent preoperative clinical swallowing assessment with a speech and language therapist (SLT). A preoperative clinical and instrumental evaluation allows determination of the patient’s baseline abilities, which are crucial for planning of targeted postoperative rehabilitation. Patients after TAGS are assessed postoperatively only in case of impaired swallowing and speech.
Postoperative management
The indications for adjuvant treatment(s) (radiotherapy, RT/chemoradiotherapy, CRT) were determined based on the NCCN guidelines and discussed by a multidisciplinary team during a tumour board.
For patients undergoing major surgery (CTS or EG), daily postoperative swallowing rehabilitation, guided by a dedicated SLT, began at the patient’s bedside in the postoperative period (from the seventh postoperative day, unless surgical or medical complications occurred). After discharge, patients continued swallowing rehabilitation in outpatient services.
Assessment of functional outcomes and quality of life
The functional swallowing outcome was assessed through the administration of questionnaires on swallowing function and quality of life (QoL) between 6 months and 1 year postoperatively or after the end of adjuvant therapy. The Italian version of the Functional Oral Intake Scale (FOIS) 15 was used to evaluate patients’ oral feeding status. Additionally, patients were asked to indicate the types of consistencies of foods and liquids they could take orally, categorised according to the International Dysphagia Diet Standardisation Initiative (IDDSI) Framework of 2016 16. QoL was assessed using the Eating Assessment Tool (EAT-10) 17 and the MD Anderson Dysphagia Inventory (MDADI) 18.
Statistical analysis
The data were analysed using IBM SPSS Statistics Version 27.
A descriptive analysis of continuous variables (mean, median, standard deviation) was conducted. For inferential analysis, a Student’s t-test was used to compare means for normally distributed variables, a Mann-Whitney U Test for comparing independent variables within the same group of patients, and ANOVA for the comparison of means in the presence of multiple variables. Furthermore, a multivariate analysis of covariance (ANCOVA) was conducted, with the classification of glossectomies as the dependent variable and patient age along with ASA score as covariates.
A p-value less than 0.05 was considered statistically significant.
Results
A total of 92 patients with OTFOMSCC who met the inclusion criteria were enrolled: 44 patients underwent TAGS for early-stage tumours, and 48 underwent major surgery for advanced stage tumours. Among these latter 48 patients: 35 underwent CTS, 3 underwent EG Type A, 6 underwent EG Type B, and 4 underwent EG Type C.
The demographic and oncological characteristics of the study population are reported in Table I.
The previous treatments on the oral cavity received by patients treated with major surgery are summarised in Table II.
In patients undergoing TAGS, healing of the defect always occurred by second intention, covering the defect with an artificial matrix (Tachosil).
In patients undergoing major surgery, concurrent reconstruction of the surgical defect was performed using a free or pedicled flap. The types of flaps used, depending on the surgical approach, are reported in Table III.
Among these, 33 patients underwent the procedure via pull-through, while 15 required mandibulotomy (including 11 CTS, 3 EG Type B, and 1 EG Type C) due to trismus or tumour of the posterior tongue or because they required concurrent segmental mandibular resection.
The majority of OTFOMSCC originated from the mobile tongue (68 patients) and the floor of the mouth (14 patients). In the remaining cases, there was involvement of both the lingual margin and the floor of the mouth (5 patients) or both the base of the tongue and the lingual margin (1 patient) without a clear origin of onset since they were already in an advanced stage (Tab. IV).
Regarding the involvement of adjacent structures by advanced OTFOMSCC, the following sites were affected:
- mandible in 4 CTS, one EG Type B, and one EG Type C. In 3 CTS and EG Type B, marginal mandibular resection was performed, while in two patients, segmental resection was carried out. In a patient undergoing CTS and one undergoing EG Type C, hemimandibulectomy was performed, requiring not only an anterolateral thigh (ALT) flap, but also a reconstructive plate;
- oropharynx with resection of the base of the tongue and ipsilateral tonsil in 10 CTS, one EG Type A, and one EG Type B (in the latter, resection was extended to include the lateral pterygoid muscle due to suspected intraoperative infiltration);
- soft palate in 2 CTS and 1 EG Type A;
- a lateral portion of the hyoid bone was resected in a patient undergoing EG Type A.
Minor complications were observed in 3 patients (CTS): one lateral neck abscess and two orocutaneous fistulas, which resolved with conservative treatments and antibiotic therapy. Complications requiring surgical revision in the operating room were observed in 6 patients undergoing CTS: two haemostasis revisions, one surgical wound revision for a lateral neck abscess, partial necrosis of the anterolateral thigh free flap (ALTF) requiring revision of the anastomosis, and two cases of ALTF necrosis replaced with a buccinator myo-mucosal flap or a pectoralis major myo-cutaneous flap (PMMC). No surgical complications occurred at the donor site.
In all patients, the tracheostomy tube was removed after surgery (mean time of tracheostomy dependence, 8 days). At follow-up between 6 months and 1 year after surgery or end of adjuvant therapy, 5 patients remained dependent on gastrostomy (1 CTS and 1 EG Type A extended to the oropharynx and soft palate, 1 EG Type B in a patient with compromised mental status, 2 EG Type C).
Functional outcomes
SWALLOWING
Regarding the functional swallowing results, data from 92 patients were collected. The median FOIS score at follow-up after minimum 6 months from surgery was 7 in TAGS, 6 in CTS, 6 in EG Type A, 5.5 in EG Type B, and 2 in EG Type C. The difference between these groups was statistically significant (p = 0.000), with a progressive worsening as the complexity of the surgical resection increased.
Regarding the percentage of patients who managed to resume oral feeding for various consistencies it was measured with the IDDSI scale (Tab. V). All patients undergoing TAGS were able to resume oral feeding with all consistencies up to IDDSI 6. Regarding IDDSI 7, the result was possible in 41 of a total of 44 patients. Regarding the CTS group, only one patient had difficulty with the intake of pure liquids, but all patients achieved the goal of consuming a semisolid and semiliquid diet (IDDSI 1-4). The majority of patients reached an IDDSI 6 diet (86%) and 23% an IDDSI 7 diet.
Regarding EG, a clear decline in performance was observed from Type A to Type C. In EG Type A, all patients managed to consume a liquid, semiliquid, and semisolid diet (IDDSI 0-4). The majority of patients (67%) also regained a soft consistency, while only one-third of patients have an unrestricted diet (Fig. 1).
In EG Type B, all patients can manage consistencies up to IDDSI 2, two-thirds of the patients handle the semi-solid consistency (IDDSI 3-4), and half of the patients can regularly consume a soft diet, while no patient succeeded in achieving a diet without limitations.
Regarding EG Type C, all patients can intake semi-liquid food orally (IDDSI 1-2), while only one patient managed to feed on a semi-solid and soft diet during rehabilitation (IDDSI 3-6).
QUALITY OF LIFE
Questionnaires regarding QoL were administered to a total of 92 patients, including those undergoing transoral surgery and major surgeries. The difference among various subgroups (TAGS, CTS, EG Types A, B, and C) regarding both the EAT-10 score and the scores of the MDADI composite and global scales was statistically significant (p = 0.000), with a progressive worsening of scores as the resected anatomical unit increased. The distribution of values for the FOIS scale and the EAT-10, MDADI global, and composite questionnaires can be observed in the follow-up conducted over a period exceeding 6 postoperative months (Figs. 2-3).
ANALYSIS OF PROGNOSTIC FACTORS ON SWALLOWING OUTCOME AND QoL
A univariate analysis was conducted evaluating the tumour site as a possible influencing factor on functional outcomes, dividing patients into subgroups (lingual margin, oral floor, posterior third of the tongue). The difference in scores obtained in all scales and questionnaires, in subgroups divided by tumour site, did not result of statistical significance: FOIS p = 0.220; EAT-10 p = 0.164; MDADI global p = 0.154; MDADI composite p = 0.310.
Therefore, we performed prognostic factor analyses on functional outcomes in the subgroup of patients undergoing CTS (35 patients). We performed univariate analysis to evaluate how the extension of the disease and surgical resection in the mandible, oropharynx, and soft palate affected functional outcomes, as measured by FOIS, and impact on QoL, assessed through EAT-10 and MDADI questionnaires. The same analysis was carried out regarding the surgical approach, whether performed through mandibulotomy or pull-through. The results are shown in Table VI. The only significant findings were observed in the FOIS (p = 0.000) and EAT-10 questionnaire (p = 0.002), specifically regarding the extension to the soft palate, where a notable decline was observed when excision of the soft palate became necessary. In the EAT-10 questionnaire (p = 0.003) and MDADI composite (p = 0.009), significant results were found regarding adjuvant therapy, with a worsening of functionality and QoL in patients undergoing adjuvant radiotherapy or chemoradiation compared to those undergoing surgery alone. The surgical approach through pull-through or mandibulotomy, on the other hand, did not emerge as a influencing factor in swallowing or QoL outcomes.
Finally, a multivariate ANCOVA was conducted, considering the classification of glossectomies (TAGS, CTS, EG Types A, B, and C) as the dependent variable, with patient age and ASA score as covariates. Regarding the FOIS, the difference in scores was found to be significant across various groups based on the type of glossectomy (p = 0.015), independent of age or ASA score covariates.
For EAT-10, the difference in scores among different glossectomy groups was significant in univariate analysis (p = 0.000). In multivariate analysis, the EAT-10 score was correlated with the patient’s age covariate (p = 0.001) and independent of the ASA score.
The MDADI global score showed significant differences among groups in univariate analysis. However, this result was not confirmed in multivariate analysis, where statistical significance was not achieved (p = 0.229).
Conversely, the MDADI composite score exhibited significant differences among groups in both univariate and multivariate analyses (p = 0.025), but it was influenced by age covariate (p = 0.001) and ASA score (p = 0.04).
Discussion
The anatomically guided approach for OTFOMSCC entails tailoring the surgical resection based on the muscular structures involved. For cT1-T2 tumours involving only intrinsic musculature, the approach utilised in our institution is transoral tumour resection with concurrent exploration and removal of the TNT (TAGS) and direct control of the deep margin of the neoplasm through the sectioning of the hyoglossus muscle and exploration of the paramedian septum between the genioglossus and hyoglossus. For more advanced cT3-T4 tumours deeply involving extrinsic musculature or cT2 with nodal involvement, compartmental emiglossopelvectomy (CTS) in block with neck lymph nodes and the TNT is indicated. The concept of CTS is conceived to plan the removal of OTFOMSCC not based on tumour margins, but on the anatomical boundaries of the so-called “oncological compartment”. This approach is grounded in previous studies conducted by Calabrese and colleagues, demonstrating a predictable progression pattern of the tumour 8-9,12,19,20. In more advanced cases, the surgical approach is extended based on the structures of the contralateral tongue involved: intrinsic musculature for EG Type A, contralateral genioglossus for EG Type B, and the entire contralateral hemitongue in the EG Type C. The defect resulting from these different approaches is well predictable and measurable, given that it is based on the precise identification of all the involved muscular structures of the tongue. The primary challenge of surgery is to achieve oncological radicality while simultaneously ensuring acceptable functional outcomes. The defect size increases with the complexity of the surgery and, proportionally, the rehabilitative challenges grow to restore adequate swallowing function and an acceptable QoL. This study aimed to objectively and subjectively characterize the 5 types of glossectomies, based on the anatomical concepts described to date.
Our results demonstrate that the functional swallowing outcome is related to the type of surgery performed and is highly predictable and repeatable. Regarding long-term resumption of oral feeding, the group of patients undergoing TAGS achieved complete rehabilitation with an unrestricted diet. Excellent swallowing results were also obtained in the CTS group. All patients consume semi-solid consistencies (IDDSI from 0 to 4), and the vast majority (86%) of patients can eat a soft diet (IDDSI 6) and 23% a regular diet (IDDSI 7) without restrictions. These excellent swallowing outcomes can be explained by careful preservation of all extrinsic muscles of the contralateral tongue, allowing a more accurate reconstruction with attachment of the reconstructive flap to a fully functional contralateral hemitongue.
In contrast, in EG cases, there was a progressive decline in swallowing performance, which remains good for EG Type A and acceptable for EG Type B, but undergoes a drastic decrease in EG Type C, confirming the extreme difficulty in rehabilitating patients undergoing total glossectomy. However, the results emphasise the importance of preserving a functional base tongue unit, the so-called hyo-styloglossus unit (HSU) when oncologically feasible, given the clear difference in outcomes between EG Type B and C.
The FOIS scale was utilised to determine a patient’s oral feeding status, as it reflects the safety and efficiency of swallowing objectified through FEES and nutritional status 15,21. The findings regarding the study of oral consistencies align with the results obtained from the FOIS scale. Our data reveal a progressive decline in FOIS scores as the surgical complexity increases. This underlines how the removal of a greater number of functional units results in a gradual decline of swallowing functionality.
Concerning the evaluation of perceived QoL following different types of glossectomies, the EAT-10 17,22,23 and MDADI 18,24-26 questionnaires were employed. The difference of the scores obtained with the EAT-10 questionnaire among patient subgroups was statistically significant (p = 0.000) and there was a progressive worsening of outcomes with increasing surgical complexity. Regarding MDADI, the difference in scores obtained among the various subgroups undergoing major surgery (CTS, EG Type A, EG Type B, and EG Type C) was statistically significant for both MDADI global and composite scores (p = 0.000). The MDADI questionnaire considers various aspects of the patient’s life. It consists of 19 items + 1 (MDADI global score) and encompasses the physical, emotional, and functional subscales reflecting specific areas of swallowing capacity perceived by the patient 25. This questionnaire was also utilised by Chepeha and colleagues 26, who recently published a study on functional outcomes and QoL of patients undergoing four types of glossectomies, performed using the classical wide-margin technique. That study also highlighted a worsening of scores with increasing complexity of resection. In particular, the authors observed a 10-point decrease in MDADI questionnaire scores between the group undergoing emiglossectomy and the group undergoing extended emiglossectomy, achieving a clinically significant difference 25.
In our study, we further evaluated the tumour’s site of onset as a possible influencing factor on functional outcomes. The difference in scores on the FOIS scale and the EAT-10, MDADI global, and composite questionnaires was not statistically significant either at discharge for the major surgery group (48 patients) or between 6 months-1 year after surgery or the end of adjuvant therapy, including TAGS (92 patients). These data are particularly important as they highlight the key concept underlying CTS, which is not based on the tumour’s site of onset but on the concept of the “oncological compartment” 8,9. The surgical defect obtained is therefore predictable for all subsites and varies only based on the infiltration of the extrinsic musculature. In contrast, in wide-margin surgery, the tumour’s location is crucial, as the resection is based on the tumour’s dimensions, which is removed at a distance of 1.5-2 cm. In the CTS subgroup, we conducted univariate analyses on potential factors influencing long-term functional outcomes. EGs were not considered due to the small sample size, and mainly because, for Types B and C, the surgical technique involves extensive destruction of the lingual body, which is not functionally comparable to “standard” CTS.
The extension of surgery to the mandible and oropharynx did not result in a significant difference in FOIS, EAT-10, and MDADI scores, both global and composite. This can be explained by the ability to effectively reconstruct defects in both the oropharynx and mandible using either free or pedicled flaps. The same rationale applies to the mandibulotomy or pull-through approach. In this case as well, a statistically significant difference was not obtained. However, regarding the extension to the soft palate, statistically significant results were obtained in both the FOIS scale (p = 0.000) and the EAT-10 questionnaire (p = 0.002). In glossectomies, a critical element of the reconstruction process is reinstating the volume that has been removed to aid swallowing by establishing contact between the tongue and the palate 26. If the resection extends to the soft palate, left unreconstructed, the neo-tongue is unable to fulfil the functions of both the base of the tongue and the palate simultaneously. This complexity poses challenges in managing the bolus during the oral and pharyngeal phases.
Also, regarding adjuvant therapy, univariate analysis to assess its impact on functional swallowing was conducted. A significant difference in the scores of the EAT-10 (p = 0.003) and MDADI composite (p = 0.009) questionnaires was observed. Adjuvant radiotherapy is an essential component in treating high-risk patients for recurrence, and the detrimental effects of radiotherapy on swallowing function are well-documented in the literature 27. In a study by Grammatica et al. 10, adjuvant therapy emerged as one of the key variables influencing functional outcomes. They conclude that subclinical food aspiration and vallecular pocket are present in a significant percentage of patients, especially when adjuvant treatments are administered.
As shown in a study by Grammatica et al. 28 on elderly patients with different comorbidities (ASA 3-4), the reconstruction with free laps of defects in the oral cavity is possible in selected patients, achieving good oncological and functional results and with good flap success rates. In our study, age and ASA score were also not negative prognostic factors for the success of reconstructive surgery. The results of multivariate analysis, considering surgical approach, age, and ASA, reveal differences among the various questionnaires. Specifically, scores obtained for FOIS and MDADI global do not appear to be influenced by patient age or ASA score. On the other hand, scores obtained for EAT-10 seem to be influenced by age (p = 0.001), and scores obtained for MDADI composite are influenced by both age (p = 0.001) and ASA score (p = 0.04). These differences can be attributed to an intrinsic distinction among the various tests used, particularly MDADI composite, which takes into account the physical, emotional, and functional subscales reflecting specific areas of swallowing capacity perceived by the patient.
The study by Grammatica et al. 10 is currently the only one in the literature describing functional outcomes, in terms of both swallowing and phonation, of CTS. However, our study analysed swallowing outcomes not only of the “standard” CTS, but also of all glossectomies performed according to the “oncologic compartment” principle and potential pathways of tumour spread. By standardising the surgical approach, modulated based on disease extension similar to what is described for open partial horizontal laryngectomies (OPHL) 29-31, it is possible to predict the surgical defect and, consequently, the functional result.
One of the main criticisms of CTS is that it is a highly aggressive approach, causing excessive loss of swallowing function 10. Our study demonstrates the fundamental importance of pursuing a modular, anatomy-guided approach to achieve not only better oncological outcomes, but also improved functional recovery and ultimately a better QoL. Patients undergoing TAGS achieve complete resumption of feeding and excellent QoL, and the CTS group also achieved excellent functional results.
This study further shows how these results gradually worsen when the genioglossus muscles are involved bilaterally or when total glossectomy becomes necessary for oncological reasons. The study results highlight the importance of preserving, when oncologically safe, at least one functional unit of the base of the tongue, including the HSU 32,33. The advantage of this technique is certainly represented by its reproducibility: a standardised resection, in fact, leads to a predictable reconstruction and, consequently, an equally predictable functional result.
These surgical aspects, coupled with appropriate swallowing rehabilitation, yield satisfactory long-term postoperative outcomes, encompassing both swallowing functionality and its associated QoL.
The principal constraints of this study lie in its monocentric and retrospective design. Additionally, there is a noteworthy discrepancy in sample sizes among the different groups. While the quantification of orally assumable consistencies represents a highly objective parameter, functional and QoL outcomes are influenced by inherent subjectivity within the questionnaires and subjective factors unique to individual patients. These factors are not always easily quantifiable and can impact the functional result regardless of the surgical approach. Future prospective studies may be desirable in order to confirm the result of this retrospective study.
Conclusions
Following an anatomically-guided approach to the resection of OTFOMSCC allows modulation of surgery based on the structures involved by the tumour, while preserving the functionality of the remaining units. TAGS yields functional outcomes comparable to those before the intervention. Even patients undergoing CTS can achieve excellent functional results. However, expanding the resection to involve the contralateral hemitongue results in a progressive deterioration of swallowing function, necessitating appropriate reconstruction and dedicated training with a SLT in order to achieve an acceptable QoL for these patients.
Acknowledgements
The authors would like to thank the SLT colleagues Monika Bernard, Vanessa Trevisani and Sandra Zingerle of the Speech and Language Therapy Department of the Hospital of Bolzano.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
LG, VD, AC: conceived the study, collected the data and wrote the paper; FV: performed the statistical analysis of the study; LC: conceived the study and corrected the paper.
Ethical consideration
This study was approved by the Provincial Ethics Committee of Bolzano (Protocol No. 0023477-BZ).
The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
Written informed consent was obtained from each participant/patient for study participation and data publication.
History
Received: April 11, 2024
Accepted: July 10, 2024
Figures and tables
Figure 1. Percentages of patients who succeeded in achieving oral intake of different consistencies measured using the IDDSI classification.
Figure 2. Distribution of FOIS, EAT-10, MDADI global, and composite results at follow-up between 6 months and 1 year postoperatively or after the end of adjuvant therapy in the entire cohort of patients (N = 92).
Figure 3. Schematic representation depicting the average values of FOIS, EAT-10, MDADI global, and composite results during the follow-up period, which occurred between 6 months and 1 year postoperatively or after the end of adjuvant therapy, in the total patient group comprising 92 patients.
| TAGS | CTS | EG Type A | EG Type B | EG Type C | Total | |
|---|---|---|---|---|---|---|
| No. of patients | 44 | 35 | 3 | 6 | 4 | 92 |
| M | 24 (54.5%) | 23 (65.7%) | 2 (66.7%) | 5 (83.3%) | 1 (25%) | 55 (59.8%) |
| F | 20 (45.5%) | 12 (34.3%) | 1 (33.3%) | 1 (16.7%) | 3 (75%) | 37 (40.2%) |
| Mean age | 59.6 | 64.2 | 58.7 | 51 | 60 | 60.7 |
| SD 12.8 | SD 10.3 | SD 13.9 | SD 21.9 | SD 14.4 | SD 12.9 | |
| ASA 1-2 | 38 (86.4%) | 24 (68.6%) | 2 (66.7%) | 4 (66.7%) | 3 (75%) | 71 (77.2%) |
| ASA 3-4 | 6 (13.6%) | 11 (31.4%) | 1 (33.3%) | 2 (33.3%) | 1 (25%) | 21 (22.8%) |
| cT (VIII Ed.) | ||||||
| 1 | 17 (38.6%) | 0 | 0 | 0 | 0 | 17 (18.5%) |
| 2 | 27 (61.4%) | 6 (17.1%) | 0 | 0 | 0 | 33 (35.9%) |
| 3 | 0 | 22 (62.9%) | 1 (33.3%) | 0 | 1 (25%) | 24 (26.1%) |
| 4a | 0 | 6 (17.1%) | 2 (66.7%) | 6 (100%) | 3 (75%) | 17 (18.5%) |
| 4b | 0 | 1 (2.9%) | 0 | 0 | 0 | 1 (1%) |
| cN (VIII Ed.) | ||||||
| 0 | 44 (100%) | 17 (48.6%) | 1 (33.3%) | 3 (50%) | 1 (25%) | 66 (71.4%) |
| 1 | 0 | 4 (11.4%) | 1 (33.3%) | 0 | 0 | 5 (5.4%) |
| 2a | 0 | 2 (5.7%) | 0 | 0 | 0 | 2 (2.3%) |
| 2b | 0 | 6 (17.1%) | 0 | 1 (16.7%) | 0 | 7 (7.7%) |
| 2c | 0 | 4 (11.4%) | 0 | 1 (16.7%) | 2 (50%) | 7 (7.7%) |
| 3a | 0 | 1 (2.9%) | 0 | 0 | 0 | 1 (1.1%) |
| 3b | 0 | 1 (2.9%) | 1 (33.3%) | 1 (16.7%) | 1 (25%) | 4 (4.4%) |
| Neck dissection | ||||||
| Ipsilateral | 24 (54.5%) | 30 (85.7%) | 1 (33.3%) | 1 (16.7%) | 0 | 56 (60.9%) |
| Bilateral | 0 | 4 (11.4%) | 1 (33.3%) | 1 (16.7%) | 3 (75%) | 12 (13.1%) |
| Contralateral | 0 | 1 (2.9%) | 0 | 0 | 0 | 1 (1%) |
| Not performed | 20 (45.5%) | 0 | 1 (33.3%) | 1 (16.7%) | 1 (25%) | 23 (25%) |
| pT (VIII Ed.) | ||||||
| 1 | 14 (31.8%) | 0 | 0 | 0 | 0 | 14 (15.2%) |
| 2 | 29 (65.9%) | 9 (25.7%) | 0 | 0 | 0 | 38 (41.3%) |
| 3 | 1 (2.3%) | 21 (60%) | 2 (66.7%) | 4 (66.7%) | 2 (50%) | 30 (32.6%) |
| 4a | 0 | 5 (14.3%) | 0 | 2 (33.3%) | 2 (50%) | 9 (9.8%) |
| 4b | 0 | 1 (33.3%) | 0 | 0 | 1 (1.1%) | |
| pN (VIII Ed.) | ||||||
| 0 | 16 (36.4%) | 20 (57%) | 1 (33.3%) | 2 (33.3%) | 1 (25%) | 40 (43.5%) |
| 1 | 4 (9%) | 5 (14.3%) | 0 | 0 | 0 | 9 (9.8%) |
| 2a | 0 | 1 (2.9%) | 0 | 0 | 0 | 1 (1.1%) |
| 2b | 3 (6.8%) | 1 (2.9%) | 0 | 0 | 0 | 4 (4.3%) |
| 2c | 0 | 1 (2.9%) | 1 (33.3%) | 1 (16.7%) | 0 | 3 (3.3%) |
| 3a | 0 | 0 | 0 | 0 | 0 | 0 |
| 3b | 1 (2.3%) | 7 (20%) | 0 | 2 (33.3%) | 2 (50%) | 12 (13%) |
| N/V | 20 (45.5%) | 0 | 1 (33.3%) | 1 (16.7%) | 1 (25%) | 23 (25%) |
| Mean pDOI (mm) | 5.4 | 13.4 | 13.5 | 20.8 | 31.5 | |
| SD 2.8 | SD 6 | SD 5 | SD 5.4 | SD 9.1 | ||
| Adjuvant therapy | ||||||
| None | 41 (93.2%) | 15 (42.9%) | 0 | 4 (66.7%) | 0 | 60 (65.2%) |
| RT | 2 (4.5%) | 12 (27.3%) | 1 (33.3%) | 0 | 2 (50%) | 17 (18.5%) |
| CT | 0 | 0 | 0 | 0 | 0 | 0 |
| RT-CT | 1 (2.3%) | 8 (22.9%) | 2 (66.7%) | 2 (33.3%) | 2 (50%) | 15 (16.3%) |
| pDOI: pathologic depth of invasion; RT: radiotherapy; CT: chemotherapy; RT-CT: radiochemotherapy; SD: standard deviation. | ||||||
| Previous treatments | CTS | EG | EG | EG | Total |
|---|---|---|---|---|---|
| Type A | Type B | Type C | |||
| Transoral surgery | 4 (11.4%) | 1 (33.3%) | 0 | 0 | 5 (10.4%) |
| Transoral surgery + RT | 0 | 0 | 1 (16.7%) | 0 | 1 (2%) |
| Transoral surgery + RT-CT | 0 | 0 | 1 (16.7%) | 0 | 1 (2%) |
| Contralateral | |||||
| CTS | 0 | 0 | 0 | 1 (25%) | 1 (2%) |
| RT: radiotherapy; RT-CT: chemoradiotherapy. | |||||
| CTS | EG | EG | EG | Total | |
|---|---|---|---|---|---|
| Type A | Type B | Type C | |||
| ALTF | 25 (71.4%) | 3 (100%) | 5 (83.3%) | 3 (75%) | 36 (75%) |
| RFFF | 7 (20%) | 0 | 0 | 0 | 7 (14.6%) |
| PMMC | 1 (2.9%) | 0 | 1 (16.7%) | 1 (25%) | 3 (6.2%) |
| Platysma flap | 2 (5.8%) | 0 | 0 | 0 | 2 (4.2%) |
| ALTF: anterolateral thigh flap; RFFF: radial forearm free flap; PMMC: pectoralis major myo-cutaneous flap. | |||||
| Sites | TAGS | CTS | EG | EG | EG | Total |
|---|---|---|---|---|---|---|
| Type A | Type B | Type C | ||||
| Lingual margin | 41 (93.2%) | 19 (54.3%) | 2 (66.7%) | 4 (66.8%) | 2 (50%) | 68 (73.9%) |
| FOM | 3 (6.8%) | 8 (22.9%) | 1 (33.3%) | 1 (11.6%) | 1 (25%) | 14 (15.3%) |
| Posterior third of the tongue | 0 | 4 (11.4%) | 0 | 0 | 0 | 4 (4.3%) |
| Lingual margin + FOM | 0 | 4 (11.4%) | 0 | 0 | 1 (25%) | 5 (5.4%) |
| Lingual margin + posterior third of the tongue | 0 | 0 | 0 | 1 (11.6%) | 0 | 1 (1.1%) |
| FOM: floor of the mouth. | ||||||
| TAGS | CTS | EG-A | EG-B | EG-C | |
|---|---|---|---|---|---|
| Liquid (IDDSI 0) | 44/44 (100%) | 34/35 (97%) | 3/3 (100%) | 5/6 (83%) | 1/4 (25%) |
| Semi-liquid (IDDSI 1-2) | 44/44 (100%) | 35/35 (100%) | 3/3 (100%) | 6/6 (100%) | 4/4 (100%) |
| Semi-solid (IDDSI 3-4) | 44/44 (100%) | 35/35 (100%) | 3/3 (100%) | 4/6 (67%) | 1/4 (25%) |
| Soft (IDDSI 5-6) | 44/44 (100%) | 30/35 (86%) | 2/3 (67%) | 3/6 (50%) | 1/4 (25%) |
| No restriction diet (IDDSI 7) | 41/44 (93%) | 8/35 (23%) | 1/3 (33%) | 0/6 (0%) | 0/4 (0%) |
| FOIS | EAT-10 | MDADI global | MDADI composite | |
|---|---|---|---|---|
| Involvement of other structures | 0.880 | 0.501 | 0.046 | 0.16 |
| Involvement of mandible | 0.492 | 0.394 | 0.452 | 0.377 |
| Tonsil | 0.841 | 0.840 | 0.087 | 0.106 |
| Soft palate | 0.000 | 0.002 | 0.224 | 0.160 |
| Mandibulotomy or pull-through | 0.191 | 0.437 | 0.152 | 0.079 |
| Adjuvant therapy (RT/RT-CT) | 0.897 | 0.003 | 0.363 | 0.009 |
| RT: radiotherapy; RT-CT: chemoradiotherapy. Statistically significant results are in italics. | ||||
References
- Sung H, Ferlay J, Siegel R. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209-249. doi:https://doi.org/10.3322/caac.21660
- Gazzini L, Fazio E, Dallari V. Impact of the COVID-19 pandemic on head and neck cancer diagnosis: data from a single referral center, South Tyrol, Northern Italy. Eur Arch Otorhinolaryngol. 2022;279:3159-3166. doi:https://doi.org/10.1007/s00405-021-07164-y
- Calabrese L, Tagliabue M, Grammatica A. Compartmental tongue surgery for intermediate-advanced squamous cell carcinoma: a multicentric study. Head Neck. 2023;45:2862-2873. doi:https://doi.org/10.1002/hed.27517
- Calabrese L, Giugliano G, Bruschini R. Compartmental surgery in tongue tumours: description of a new surgical technique. Acta Otorhinolaryngol Ital. 2009;29:259-264.
- Calabrese L, Tagliabue M, Maffini F. From wide excision to a compartmental approach in tongue tumors: what is going on?. Curr Opin Otolaryngol Head Neck Surg. 2013;21:112-117. doi:https://doi.org/10.1097/MOO.0b013e32835e28d2
- Tagliabue M, Gandini S, Maffini F. The role of the T-N tract in advanced stage tongue cancer. Head Neck. 2019;41:2756-2767. doi:https://doi.org/10.1002/hed.25761
- Grammatica A, Piazza C, Ferrari M. Step-by-step cadaver dissection and surgical technique for compartmental tongue and floor of mouth resection. Front Oncol. 2021;11. doi:https://doi.org/10.3389/fonc.2021.613945
- Calabrese L, Bruschini R, Giugliano G. Compartmental tongue surgery: long term oncologic results in the treatment of tongue cancer. Oral Oncol. 2011;47:174-179. doi:https://doi.org/10.1016/j.oraloncology.2010.12.006
- Piazza C, Grammatica A, Montalto N. Compartmental surgery for oral tongue and floor of the mouth cancer: oncologic outcomes. Head Neck. 2019;41:110-115. doi:https://doi.org/10.1002/hed.25480
- Grammatica A, Piazza C, Montalto N. Compartmental surgery for oral tongue cancer: objective and subjective functional evaluation. Laryngoscope. 2021;131:E176-E183. doi:https://doi.org/10.1002/lary.28627
- Calabrese L, Pietrobon G, Fazio E. Anatomically-based transoral surgical approach to early-stage oral tongue squamous cell carcinoma. Head Neck. 2020;42:1105-1109. doi:https://doi.org/10.1002/hed.26095
- Gazzini L, Fazio E, Dallari V. Beyond the boundaries of compartmental hemiglossectomy: a proposal for an anatomically based classification of surgical approaches to advanced oral tongue squamous cell carcinoma. Eur Arch Otorhinolaryngol. 2023;280:3015-3022. doi:https://doi.org/10.1007/s00405-023-07915-z
- Brierley J, Gospodarowicz M, Wittekind C. TNM Classification of Malignant Tumors. Wiley-Blackwell; 2016.
- Gazzini L, Dallari V, Fazio E. How I do it: transoral surgical approach to early-stage oral tongue squamous cell carcinoma (with video). Eur Ann Otorhinolaryngol Head Neck Dis. 2021;138:45-46. doi:https://doi.org/10.1016/j.anorl.2021.02.019
- Battel I, Calvo I, Walshe M. Cross-cultural validation of the Italian version of the functional oral intake scale. Folia Phoniatr Logop. 2018;70:117-123. doi:https://doi.org/10.1159/000490792
- Cichero J, Lam P, Steele C. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: the IDDSI framework. Dysphagia. 2017;32:293-314. doi:https://doi.org/10.1007/s00455-016-9758-y
- Belafsky P, Mouadeb D, Rees C. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117:919-924. doi:https://doi.org/10.1177/000348940811701210
- Chen A, Frankowski R, Bishop-Leone J. The development and validation of a dysphagia-specific quality-of-life questionnaire for patients with head and neck cancer: the M.D. Anderson dysphagia inventory. Arch Otolaryngol Head Neck Surg. 2001;127:870-876.
- Calabrese L, Bizzoca M, Grigolato R. From bench to bedside in tongue muscle cancer invasion and back again: gross anatomy, microanatomy, surgical treatments and basic research. Life (Basel). 2020;10. doi:https://doi.org/10.3390/life10090197
- Piazza C, Montalto N, Paderno A. Is it time to incorporate “depth of infiltration” in the T staging of oral tongue and floor of mouth cancer?. Curr Opin Otolaryngol Head Neck Surg. 2014;22:81-89. doi:https://doi.org/10.1097/MOO.0000000000000038
- Ninfa A, Pizzorni N, Eplite A. Validation of the Italian version of the Functional Oral Intake Scale (FOIS-It) against fiberoptic endoscopic evaluation of swallowing and nutritional status. Dysphagia. 2022;37:137-147. doi:https://doi.org/10.1007/s00455-021-10257-9
- Wilmskoetter J, Bonilha H, Hong I. Construct validity of the Eating Assessment Tool (EAT-10). Disabil Rehabil. 2019;41:549-559. doi:https://doi.org/10.1080/09638288.2017.1398787
- Schindler A, Mozzanica F, Monzani A. Reliability and validity of the Italian Eating Assessment Tool. Ann Otol Rhinol Laryngol. 2013;122:717-724. doi:https://doi.org/10.1177/000348941312201109
- Schindler A, Borghi E, Tiddia C. Adaptation and validation of the Italian MD Anderson Dysphagia Inventory (MDADI). Rev Laryngol Otol Rhinol (Bord). 2008;129:97-100.
- Hutcheson K, Barrow M, Lisec A. What is a clinically relevant difference in MDADI scores between groups of head and neck cancer patients?. Laryngoscope. 2016;126:1108-1113. doi:https://doi.org/10.1002/lary.25778
- Chepeha D, Esemezie A, Philteos J. Glossectomy for the treatment of oral cavity carcinoma: quantitative, functional and patient-reported quality of life outcomes differ by four glossectomy defects. Oral Oncol. 2023;142. doi:https://doi.org/10.1016/j.oraloncology.2023.106431
- Fujiki M, Miyamoto S, Zenda S. Longitudinal and long-term effects of radiotherapy on swallowing function after tongue reconstruction. J Laryngol Otol. 2016;130:865-872. doi:https://doi.org/10.1017/S0022215116008720
- Grammatica A, Piazza C, Pellini R. Free flaps for advanced oral cancer in the “Older Old” and “Oldest Old”: a retrospective multi-institutional study. Front Oncol. 2019;9. doi:https://doi.org/10.3389/fonc.2019.00604
- Succo G, Peretti G, Piazza C. Open partial horizontal laryngectomies: a proposal for classification by the working committee on nomenclature of the European Laryngological Society. Eur Arch Otorhinolaryngol. 2014;271:2489-2496. doi:https://doi.org/10.1007/s00405-014-3024-4
- Bertolin A, Lionello M, Ghizzo M. Modular approach in OPHL: are there preoperative predictors?. Acta Otorhinolaryngol Ital. 2020;40:352-359. doi:https://doi.org/10.14639/0392-100X-N0782
- Molteni G, Bertolin A, Gazzini L. Modular approach to open partial horizontal laryngectomy: step-by-step anatomic dissection. Otolaryngol Head Neck Surg. 2022;166:601-602. doi:https://doi.org/10.1177/01945998211026528
- Gazzini L, Caselli A, Dallari V. Subtotal glossectomy with conservation of the hyo-styloglossus unit (HSU): a new pivotal concept for preserving tongue function in extended glossectomy. Front Surg. 2024;11. doi:https://doi.org/10.3389/fsurg.2024.1395936
- Gazzini L, Dallari V, Fazio E. Functional tongue reconstruction after compartmental surgery: a schematic model for planning and insetting of the anterolateral thigh free flap. Eur Arch Otorhinolaryngol. Published online 2024. doi:https://doi.org/10.1007/s00405-024-08982-6
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2024 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 1569 times
- PDF downloaded - 314 times



