Head and neck
Vol. 44: Issue 6 - December 2024
Lateral hypopharyngectomy with laryngeal preservation reconstructed with inlay fasciocutaneous free flaps: clinical and functional outcomes
Abstract
Objective. Lateral hypopharyngectomy (LH) is one of the organ-preservation surgical strategies available for treatment of selected naïve early squamous cell carcinoma (SCC), as well as for rarer non-SCC tumours and persistent/recurrent/second primaries after chemoradiation of the lateral wall of the piriform sinus. Its reconstructive methods have been the subject of different approaches without a general consensus. The aim of the present study is to describe a retrospective series of LH reconstructed by inlay fascio-cutaneous free flaps, reporting on oncological and functional outcomes.
Methods. Patients who underwent LH at the Department of Otorhinolaryngology – Head and Neck Surgery of the University of Brescia, Italy, between 2017 and 2023 were retrospectively reviewed. Clinical history, tumour histotype, postoperative complications, functional, and oncological outcomes were collected.
Results. Seven patients (6 males, 1 female) were included. In all, 29% had a treatment-naïve neoplasm, while 71% had recurrent disease. The final histology included 3 SCC, 2 synovial sarcomas, one liposarcoma, and one single-site mucosal metastasis from cutaneous melanoma. Negative margins were achieved in 6 patients (86%). All patients had swallowing rehabilitation by speech therapists and were able to safely eat a free diet at discharge, except for one who needed a percutaneous endoscopic gastrostomy to support nutritional oral intake. After a mean follow-up of 34.3 months, all patients except one are alive.
Conclusions. Our study showed that, in selected cases, it is possible to radically remove lateral hypopharyngeal tumours with laryngeal preservation and free flaps inlay reconstruction, with a low rate of complications and acceptable functional and oncological results.
Introduction
According to different international guidelines, treatment options for early hypopharyngeal squamous cell carcinoma (HSCC) are either radiotherapy (RT) or partial/conservative surgical procedures 1,2. In contrast, for advanced stage lesions, a combination of different treatment modalities is always indicated. On the other hand, in case of persistent/recurrent HSCC after (chemo-)RT [(C)RT], surgery, when feasible, represents the only treatment option, and is mainly based on non-organ preservation salvage procedures, i.e. total laryngectomy (TL) extended to the hypopharynx 3, with ensuing reconstruction by pedicled myo-cutaneous, free fascio-cutaneous, or visceral flaps 4,5.
Regarding surgery in early T categories, carbon dioxide transoral laser microsurgery (CO2 TOLMS) 6 alone frequently may not be applicable due to the very low probability of finding small tumours limited to the piriform sinus, with no lymph node metastasis. The frequent loco-regional advancement of disease will, in fact, lead to the creation of a through and through defect resulting from transoral resections which, in association with ipsilateral neck dissection, will increase the risk of salivary fistula, neck infection and risk of blowout of large vessels if not properly repaired. Adjuvant treatment(s) are also more the rule than the exception. On the other hand, TL with partial or circumferential hypopharyngectomy represents a safe and standardised treatment for locally advanced cancers, but may be poorly accepted in case of limited persistence/recurrence after (C)RT or second primary in patients already irradiated in the head and neck area. Therefore, in case of early stage naïve HSCC choosing a surgical option or in presence of limited recurrence after (C)RT without arytenoid hypomobility/fixation, lateral hypopharyngectomy (LH) with laryngeal preservation may be considered a viable option. Similarly, the same may represent a valid solution in case of rarer non-SCC tumours of the piriform sinus where guidelines are definitively less defined and a personalised choice according to the patient’s profile must be embraced.
Between 1930 and 1932, Trotter with lateral pharyngotomy 7 and Orton with trans-thyroid pharyngotomy 8 provided the groundwork for hypopharyngeal surgery with laryngeal preservation, even though these procedures never achieved popularity due to the high rates of mortality and morbidity (mainly fistulas and neck infection) reported at that time. Later, Ogura et al. in 1960 9 were the first to describe the feasibility of lateral pharyngotomy with sectioning of the lateral portion of the thyroid ala and primary reconstruction. This technique was further implemented by Urken et al. 10 and Ishida et al. 11 using free flap reconstruction in order to obtain more favourable functional results. When applied with the same oncological principles of radicality (R0), LH with laryngeal preservation was demonstrated to avoid the functional sequalae of TL while still maintaining good loco-regional control.
The aim of the present study is to review a retrospective, mono-institutional series of LH reconstructed by inlay fascio-cutaneous free flaps, describing our surgical technique as well as oncological and functional outcomes.
Materials and methods
Patients who underwent LH at the Department of Otorhinolaryngology – Head and Neck Surgery of the University of Brescia, Italy, between January 2017 and December 2023 were retrospectively reviewed. Our indications for LH were: 1) unilateral hypopharyngeal lesions, centred into the lateral wall of the piriform sinus, not involving the retrocricoid region, posterior hypopharyngeal wall, and oesophageal mucosa; 2) preserved arytenoid motility, without cricoid and/or thyroid cartilage involvement; 3) HSCC and non-SCC histotypes, in particular non-radiosensitive or recurrent/second primary tumours after (C)RT; 4) good patient performance status and absence of major pulmonary, cardiovascular, or neurological comorbidities.
A dedicated database was built, including demographic data (age at presentation, gender), clinical history, preoperative imaging and staging, tumour histotype, final histopathological report, postoperative complications, functional outcomes in terms of speech and swallowing, adjuvant treatment(s), and clinical follow-up. A descriptive statistical analysis was conducted.
Surgical technique
After orotracheal intubation, ipsilateral neck dissection is carried out, based on preoperative imaging and probability of occult lymph nodes metastases. The superior laryngeal pedicle is then identified and ligated, sparing the principal trunk of the superior laryngeal nerve, in order to preserve the supraglottic sensitivity as much as possible. To gain complete control on the piriform sinus, the greater cornu of the hyoid bone is removed leaving the lesser one. Then, after incising the constrictor muscle at the level of the posterior border of the thyroid lamina, the submucosa of the piriform sinus is bluntly detached from the inner side of the cartilage itself. With the piriform sinus under direct control, the superior cornu and the postero-lateral aspect of the thyroid cartilage are removed and sent for histopathological examination, preserving the thyroid inferior cornu to protect the entry point of the recurrent laryngeal nerve. Preserving superior and inferior laryngeal nerves is fundamental to guarantee ideal functional rehabilitation and maintain supraglottic sensitivity and cricopharyngeal muscle sphincteric function. This technical detail is of paramount importance in avoiding cricopharyngeal denervation with ensuing hypertone causing swallowing difficulties.
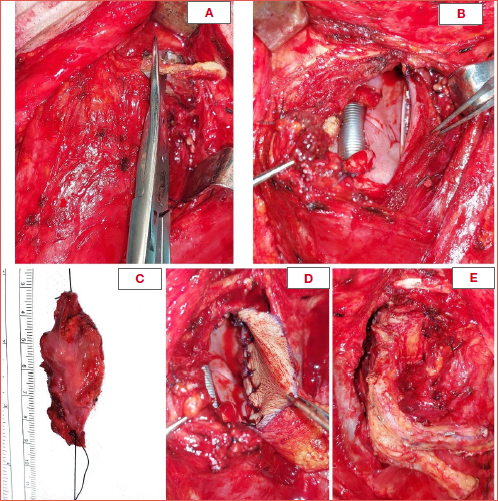
At this point, LH is carried out, entering the pharyngeal lumen just below the residual hyoid bone. Tumour resection is accomplished under direct endoluminal vision. A precise measurement of both the surgical specimen and defect is made and a defect-tailored fascio-cutaneous radial forearm free flap (RFFF) harvested, paying attention to prepare a slightly oversized skin paddle in order to improve organ mobility during swallowing and restore the three dimensions of the new piriform sinus. In addition, the length of the artery and vein are always adequately measured in order to avoid any pedicle redundancy and kinking within the neck. During the insetting of the flap, care must be addressed to suture the flap along the posterior wall of the hypopharynx, cranially to the tonsillar region and amigdalo-glossus sulcus, while antero-inferiorly to the oesophageal mucosa and soft tissues filling the paraglottic space. In this phase, to get an extra-tension of the free flap and thus prevent its excessive prolapse into the airway and digestive lumen, suture can be passed through the residual thyroid lamina and thyro-hyoid membrane with overlaying strap muscles. After accomplishment of the insetting of the flap, its revascularisation is performed by usual microsurgical techniques (Cover figure). A temporary tracheotomy and a nasogastric feeding tube are placed in all patients.
Postoperative management
Intravenous antibiotic therapy is usually administered for 8-10 days. Daily endoscopic examinations are performed to check free flap vascularisation, airway oedema, and patency. The tracheotomic cannula size is gradually reduced from 6 to 4, then plugged for increasing time during the day and night, and finally removed as soon as possible. Swallowing rehabilitation by a speech therapist starts with mobility exercises from the 3rd-4th postoperative day. After tracheostomy removal, oral feeding rehabilitation starts under speech therapist supervision, with increasing food consistencies and regular endoscopic evaluations. The nasogastric feeding tube is removed when satisfying swallowing rehabilitation is obtained. Based on the definitive histopathologic report, adjuvant treatment(s) are indicated and delivered after multidisciplinary evaluation, if appropriate.
Results
Seven patients, one female (14%) and 6 males (86%), were included in the present study. Mean age at diagnosis was 61 years (range, 36-77). Smoking habits were reported in 3 patients and one reported both smoking and alcohol abuse. All patients underwent preoperative neck CT and/or MRI and PET or thorax CT. Tumour localisation was centred in all patients at the level of the lateral wall of the piriform sinus, aryepiglottic or pharyngo-epiglottic folds, without laryngeal cartilages infiltration, and with normal laryngeal motility. No patient had clinically and/or radiologically evidence of distant metastasis. Two (29%) patients had a naïve neoplasm, while 5 (71%) had recurrent/persistent disease or a second primary in an already irradiated organ. Preoperative tumour histology was as follows: 3 (43%) SCC, 2 (29%) synovial sarcomas, one (14%) liposarcoma, and one (14%) single-site mucosal metastasis of cutaneous melanoma. In 57% of patients, ipsilateral neck dissection was performed. In all cases, final histopathological examination confirmed preoperative histology. Negative (R0) margins were achieved in 6 patients (86%) and only in one case (14%, patient with synovial sarcoma) were the margins microscopically positive (R1). Three patients (43%) underwent adjuvant treatments with (C)RT or immunotherapy. All details are reported in Table I.
The mean length of hospitalisation was 19.7 days (range, 15-25). Complications were: one bleeding treated with surgical revision under general anaesthesia and one free flap failure on the 11th postoperative day treated with reconstruction by a second (anterolateral tight [ALT]) free flap (Figs. 1a and b). No medical complications were reported. All patients had swallowing rehabilitation by speech therapists and were able to safely eat a free diet at discharge, except for one patient who needed a percutaneous endoscopic gastrostomy (PEG) to support the nutritional oral intake. No aspiration pneumonia was encountered. Decannulation was accomplished in all patients, with an average decannulation time of 10.6 days (range, 6-15). All data are reported in Table II. Mean follow-up is 34.3 months (range, 6-96). All patients are alive except for one who died 12 months after surgery for local recurrence of synovial sarcoma. Among the remaining patients, one is alive with disease at 44 months after surgery and continues immunotherapy for distant metastases of skin melanoma. Another patient underwent pulmonary partial resection for synovial sarcoma metastasis and is alive without disease at 96 months after surgery. During follow-up, no aspiration or pneumonia were reported and 6 (86%) patients had a free diet with good functional outcomes, while one (14%) continued liquid oral diet supported by PEG nutrition. Voice is rated as normal by both patients and speech therapists in all cases.
Discussion
The present paper describes the surgical technique and oncological and functional results of LH with laryngeal preservation and inlay fascio-cutaneous free flaps reconstruction in a monocentric, retrospective cohort of patients. This procedure can be ideally accounted as a viable treatment strategy for management of very selected early HSCC and non-SCC hypopharyngeal tumours, lying in between non-surgical protocols (i.e. [C]RT) and TL with partial hypopharyngectomy. The goals of LH are to obtain an adequate R0 resection, without impairing laryngeal functions and maintaining an acceptable quality of life, especially in terms of voice and swallowing. Our indications for this procedure are mainly represented by unilateral hypopharyngeal lesions, centred into the lateral wall of the piriform sinus with preserved arytenoid motility, without cricoid and/or thyroid cartilages involvement, as well as extension to the retrocricoid, posterior hypopharyngeal wall, and oesophageal mucosa. LH can be applied to both HSCC and non-SCC histotypes. In particular, this procedure may be warranted for treatment of non-radiosensitive lesions or in recurrent/second primary after (C)RT. A good performance status and absence of major pulmonary, cardiovascular or neurological comorbidities are mandatory for proper patient selection as described for other open partial horizontal laryngectomies 12-15. Ogura et al. 9 were the first to describe the feasibility of LH with sectioning of the lateral portion of the thyroid ala. The authors highlighted the importance of removing the hyoid bone in the midline and a portion of the thyroid cartilage to gain a better access to the region and thus allow tumour resection under direct vision. The reconstructive phase of the Ogura’s technique consisted in the primary suture of the base of the tongue with a perichondral thyroid flap harvested during cartilage resection or with skin graft in case of larger defects. As described by the same authors, fistulas occasionally occurred. Later, Holsinger et al. 17 described a similar approach to the hypopharynx with primary closure and, even though they reported good functional and oncological outcomes, they also encountered one perioperative death due to a salivary leak.
In order to avoid such complications, Cristalli and co-workers 16 recently reported a similar technique, which differs from that of Ogura for a limited resection of the lateral portion of the hyoid bone, and for reconstruction through a primary closure and an onlay free flap. Closure was performed by direct approximation of the posterior border of the sectioned thyroid cartilage to the posterior hypopharyngeal wall after gently mobilising it from the prevertebral fascia in association to the use of an onlay fascial antebrachial free flap, i.e. a second layer of vascularised and non-irradiated tissue aimed at reducing the risk of postoperative fistula. No postoperative complications were reported, but a moderate grade of dysphagia was noted in one-third of patients.
Urken et al. 10 were the first to describe a direct reconstruction of the piriform sinus after partial vertical laryngopharyngectomy performed with cartilage graft and sensate RFFF. Similar to our technique, Ishida 11 reported a large case series of lateral partial hypopharyngectomy with resection of the lateral half of the thyroid cartilage, vocal cord preservation and reconstruction with free flaps (38 RFFF and 16 ALT). Salivary fistula occurred in 4 patients and only one required surgical revision (primary closure).
Our technique required the section of the greater cornu of the hyoid bone, the superior cornu and the postero-lateral aspect of the thyroid cartilage to gain a complete control of the piriform sinus and perform a safe tumour resection under direct vision. We prefer to reconstruct the defect by an inlay fascio-cutaneous thin RFFF in order to perform a carefully three-dimensional tailored-defect reconstruction, reduce the fistula rate, avoid stenosis caused by primary closure, especially in the perspective of adjuvant (C)RT, and, on the other hand, to recreate a cavity that, although insensate, may reproduce the piriform sinus geometry to improve functional outcomes, in terms of oral feeding and management of secretion.
Various free flaps have been described in the literature for reconstruction after partial hypopharyngectomy 18-23,25. Julieron et al. 21 demonstrated that results of reconstruction with pectoralis myocutaneous pedicled flap were poor, primarily for its excessive skin paddle thickness and bulkiness. In contrast, one of the most widely used flaps in this field is definitely the RFFF, due to its thinness and pliability, which is particularly suitable for the reconstruction of the delicate hypopharyngeal mucosa 21,24. In the literature, good results have also been reported with free jejunal patch graft for reconstruction of defects after LH with laryngeal preservation 18,23. However, potentially life-threatening complications such as bowel anastomotic leakage, bowel obstruction, and abdominal wound dehiscence have been described 25. In all cases of the present series, our first reconstructive choice was the RFFF due to several advantages, including its thinness, rapid harvesting, variability of length based on defect, large-calibre vascular pedicle, and relatively low donor site morbidity 24, especially compared to jejunal harvest. Our fistula rate was 0% and free flap failure was observed in one patient only with ensuing harvesting of a second ALT free flap. The patient’s body habitus in this case was thin enough to allow good function even after this type of reconstruction which, in our experience, remains a second-choice option (Figs. 1A-B).
According to the literature, in case of conservative hypopharyngeal resection, tracheotomy should be always performed during the intervention 9-11,21. We also followed this principle to safely control the airways in prevision of postoperative oedema and to allow, in association with nasogastric feeding tube, complete healing of the suture line before the restart of oral feeding. Decannulation was gradually achieved, ideally from the 6th postoperative day (mean, 10.6 days; range, 6-15). Cristalli et al.16 reported decannulation after 21 days in 2 patients and after 2 months in one. In the cohort of Urken and coworkers 10, performing a more extended procedure in the form of vertical laryngectomy and partial hypopharyngectomy, decannulation required 2-3 months. However, a non-negligible postoperative functional rehabilitation was always necessary even in our series, with an average length of hospitalisation of 19.6 days (range, 15-25). At discharge, all patients except one (who remained PEG-dependent) were able to eat a nearly normal diet without signs of dysphagia or aspiration. No aspiration, pneumonia, or hypopharyngeal stricture were reported and the oral intake fully normalised within 2-3 months from the end of treatment. This result is especially notable if one considers that only 2 (28%) patients never received preoperative or adjuvant (C)RT.
Generally, laryngo-pharyngeal functions decline and rehabilitation is worse in older patients. For this reason, patient age and performance status should be considered as key selection criteria for this kind of surgery. On the other hand, as reported by Shinkzaki et al. 18, functional outcomes can be highly influenced by previous history of (C)RT, resulting less successful in previously treated patients needing longer postoperative rehabilitation. Careful patient selection is paramount for reliably predicting favourable postoperative functional and oncological outcomes.
The main limitation of the present retrospective unicentric study is represented by its small number of patients due to the strict inclusion criteria described. The diversity of histologies, on the other hand, can be considered a pro in terms of possibility to apply such a technique also to non-SCC lesions. The heterogeneity of our population, however, introduces a potential variability in terms of oncological outcomes, as different tumours might exhibit distinct responses to the same treatment. Moreover, our follow-up period ranges widely (6-96 months) and this may hamper the long-term validity of our assumptions. For these reasons, future multi-institutional prospective studies with a higher number of patients are needed to validate this surgical technique.
Conclusions
The hypopharynx represents a challenge for surgeons in balancing the need for oncological radicality and the desire to maintain a functioning larynx and a good quality of life. Our study showed that, in selected cases, it is possible to radically remove lateral hypopharyngeal tumours with laryngeal preservation and acceptable functional and oncological results. Our experience indicates that inlay RFFF is an excellent choice for LH reconstruction in most patients due to its thinness, pliability, reliability, and low donor site morbidity compared to other free flaps. The reconstruction allowed complete restoration of swallowing and optimal quality of life in most patients, with no postoperative fistula or development of stricture.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
DL, CM, CP: contributed to data collection, performed manuscript preparation and final edits and revisions; DM, AG, VR, GZ, CP: reviewed, contributed conceptually to the article and approved the submitted version.
Ethical consideration
This study was approved by the Institutional Ethics Committee of the University of Brescia (protocol number 4554).
The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
Written informed consent was obtained from each patient for study participation and data publication.
History
Received: May 12, 2024
Accepted: June 4, 2024
Published online: September 15, 2024
Figures and tables
Figure 1A-B. Patient with a single-site mucosal metastasis of cutaneous melanoma treated by left lateral hypopharyngectomy and reconstruction with inlay radial forearm free flap revised on the 11th postoperative day for necrosis with a second (anterolateral tight) free flap. The 3-year follow-up endoscopy shows an optimal functional reconstruction of the left piriform sinus without residual dysphagia.
| N° | Gender | Age | Previous treatment(s) | Histology | Site | Neck dissection | Decannulation time (days) | Hospitalization (days) | Margin status | pTNM | Adjuvant treatment | Follow-up (months) | Recurrence/metastasis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 77 | YES - surgery | Liposarcoma | AEF+ PEF | No | 7 | 15 | R0 | - | No | NED, 59 | No |
| 2 | F | 68 | N0 | Synovial sarcoma | PS | Right SND II-IV | 10 | 19 | R0 | - | RT | NED, 96 | Yes, lung (surgery) |
| 3 | M | 36 | YES - CRT + surgery | Synovial sarcoma | AEF+ PEF | No | 9 | 17 | R1 | - | No | DOD, 12 | Yes - palliative CHT |
| 4 | M | 49 | YES - surgery | Metastasis of melanoma | PS | Left SND II-V | 6 | 25 | R0 | - | Immunotherapy | AWD, 44 | Yes - immunotherapy |
| 5 | M | 69 | YES - CRT | SCC G3 | PS | Right SND III-IV-VI | 12 | 16 | R0 | T1N0 | No | NED, 16 | No |
| 6 | M | 66 | N0 | SCC G3 | AEF | Left MRND type III | 15 | 21 | R0 | T2N2b | CRT | NED, 7 | No |
| 7 | M | 62 | YES - surgery + CRT | SCC G3 | PEF | No | 15 | 25 | R0 | T1Nx | No | NED, 6 | No |
| CRT: chemoradiotherapy; RT: radiotherapy; CHT: chemotherapy; AEF: aryepiglottic fold; PEF: pharyngoepiglottic fold; PS: piriform sinus; SND: selective neck dissection; MRND: modified radical neck dissection; NED: no evidence of disease; DOD: dead of disease; AWD: alive with disease. | |||||||||||||
| Average length of hospitalisation | 19.6 days (range 15-25) |
|---|---|
| Complication | 2 (28%) |
| Bleeding | 1 (14%) |
| Free flap necrosis | 1 (14%) |
| Swallowing rehabilitation | 7 (100%) |
| Aspiration | 0 |
| Pneumonia | 0 |
| Dysphagia | 1 (14%) |
| Diet | |
| Free diet | 6 (86%) |
| Liquid diet + PEG | 1 (14%) |
| Mean time to decannulation | 10.6 days (range, 6-15) |
References
- Pfister DG, Spencer S, Adelstein D, et al. Head and neck cancers, version 2.2020, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 2020;18:873-898. https://doi.org/10.6004/jnccn.2020.0031
- Head and Neck Cancers | ESMO https://www.esmo.org/guidelines/guidelines-by-topic/head-and-neck-cancers/squamous-cell-carcinoma-of-the-head-and-neck
- Simo R, Rovira A, Townley W. Salvage treatment options after failed primary treatment of hypopharyngeal cancer. Adv Otorhinolaryngol 2019;83:135-147. https://doi.org/10.1159/000492357
- Piazza C, Taglietti V, Nicolai P. Reconstructive options after total laryngectomy with subtotal or circumferential hypopharyngectomy and cervical esophagectomy. Curr Opin Otolaryngol Head Neck Surg 2012;20:77-88. https://doi.org/10.1097/MOO.0b013e328350a5cc
- Piazza C, Bon FD, Paderno A, et al. Fasciocutaneous free flaps for reconstruction of hypopharyngeal defects. Laryngoscope 2017;127:2731-2737. https://doi.org/10.1002/lary.26705
- Remacle M, Arens C, Eldin MB, et al. Laser-assisted surgery of the upper aero-digestive tract: a clarification of nomenclature. A consensus statement of the European Laryngological Society. Eur Arch Otorhinolaryngol 2017;274:3723-3727. https://doi.org/10.1007/s00405-017-4708-3
- Trotter W. Malignant disease of the hypopharynx and its treatment by excision. Br Med J 1932;1:510-513. https://doi.org/10.1136/bmj.1.3715.510
- Orton HB. Lateral transthyroid pharyngotomy: Trotter’s operation for malignant conditions of the laryngopharynx. Arch Otolaryngol 1930;12:320-338. https://doi.org/10.1001/archotol.1930.03570010366005
- Ogura JH, Watson RK, Jurema AA. Partial pharyngectomy and neck dissection for posterior hypopharyngeal cancer. Immediate reconstruction with preservation of voice. Laryngoscope 1960;70:1523-1534. https://doi.org/10.1288/00005537-196011000-00002
- Urken ML, Blackwell K, Biller HF. Reconstruction of the laryngopharynx after hemicricoid/hemithyroid cartilage resection. Preliminary functional results. Arch Otolaryngol Head Neck Surg 1997;123:1213-1222. https://doi.org/10.1001/archotol.1997.01900110067009
- Ishida K, Kato T, Seino Y, et al. Free skin flap reconstruction after partial hypopharyngectomy with laryngeal preservation. J Plast Surg Hand Surg 2014;48:291-296. https://doi.org/10.3109/2000656X.2013.877914
- Succo G, Crosetti E. Limitations and opportunities in open laryngeal organ preservation surgery: current role of OPHLs. Front Oncol 2019;9:408. https://doi.org/10.3389/fonc.2019.00408
- Schindler A, Favero E, Capaccio P, et al. Supracricoid laryngectomy: age influence on long-term functional results. Laryngoscope 2009;119:1218-1225. https://doi.org/10.1002/lary.20172
- Gallo O, Locatello LG, Larotonda G, et al. Nomograms for prediction of postoperative complications in open partial laryngeal surgery. J Surg Oncol 2018;118:1050-1057. https://doi.org/10.1002/jso.25232
- Crosetti E, Caracciolo A, Molteni G, et al. Unravelling the risk factors that underlie laryngeal surgery in elderly. Acta Otorhinolaryngol Ital 2016;36:185-193. https://doi.org/10.14639/0392-100X-817
- Cristalli G, Ferri E, Di Maio P, et al. Lateral conservative approach for recurrent/persistent hypopharyngeal carcinoma: a case series. Eur Arch Otorhinolaryngol 2020;277:2375-2380. https://doi.org/10.1007/s00405-020-06009-4
- Holsinger FC, Motamed M, Garcia D, et al. Resection of selected invasive squamous cell carcinoma of the pyriform sinus by means of the lateral pharyngotomy approach: the partial lateral pharyngectomy. Head Neck 2006;28:705-711. https://doi.org/10.1002/hed.20375
- Shinozaki T, Hayashi R, Okano W, et al. Treatment results of 99 patients undergoing open partial hypopharyngectomy with larynx preservation. Jpn J Clin Oncol 2019;49:919-923. https://doi.org/10.1093/jjco/hyz091
- Azizzadeh B, Yafai S, Rawnsley JD, et al. Radial forearm free flap pharyngoesophageal reconstruction. Laryngoscope 2001;111:807-810. https://doi.org/10.1097/00005537-200105000-00010
- Disa JJ, Pusic AL, Hidalgo DA, et al. Microvascular reconstruction of the hypopharynx: defect classification, treatment algorithm, and functional outcome based on 165 consecutive cases. Plast Reconstr Surg 2003;111:652-660; discussion 661-663. https://doi.org/10.1097/01.PRS.0000041987.53831.23
- Julieron M, Kolb F, Schwaab G, et al. Surgical management of posterior pharyngeal wall carcinomas: functional and oncologic results. Head Neck 2001;23:80-86. https://doi.org/10.1002/1097-0347(200102)23:2<80::aid-hed1002>3.0.co;2-3
- Lydiatt WM, Kraus DH, Cordeiro PG, et al. Posterior pharyngeal carcinoma resection with larynx preservation and radial forearm free flap reconstruction: a preliminary report. Head Neck 1996;18:501-505. https://doi.org/10.1002/(SICI)1097-0347(199611/12)18:6<501::AID-HED3>3.0.CO;2-6
- Miyamoto S, Sakuraba M, Asano T, et al. Free jejunal patch graft for reconstruction after partial hypopharyngectomy with laryngeal preservation. Arch Otolaryngol Head Neck Surg 2011;137:181-186. https://doi.org/10.1001/archoto.2010.245
- Anthony JP, Singer MI, Deschler DG, et al. Long-term functional results after pharyngoesophageal reconstruction with the radial forearm free flap. Am J Surg 1994;168:441-445. https://doi.org/10.1016/s0002-9610(05)80095-9
- Reece GP, Bengtson BP, Schusterman MA. Reconstruction of the pharynx and cervical esophagus using free jejunal transfer. Clin Plast Surg 1994;21:125-136.
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2024 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 1318 times
- PDF downloaded - 309 times



