Rhinology
Vol. 44: Issue 4 - August 2024
TIM-3-driven macrophage polarisation is associated to recalcitrant chronic rhinosinusitis with nasal polyps
Abstract
Objective. This study evaluated the expression of TIM-3 and its influence on macrophage polarisation in recalcitrant chronic rhinosinusitis with nasal polyps (CRSwNP).
Methods. We detected TIM-3 expression in serum and tissue samples of healthy controls (HC), primary CRSwNP, and patients with recurrent CRSwNP. Macrophage markers were detected among three groups, and their correlations with TIM-3 levels were examined. Macrophages from circulating blood were collected and used to examine the impact of TIM-3 on polarisation in vitro.
Results. TIM-3 levels were enhanced in the CRSwNP group compared to the HC group. Tissue immunofluorescence revealed elevated TIM-3 expression in patients with CRSwNP, and patients with multiple recurrences exhibited higher TIM-3 levels compared to their first recurrence and baseline levels. Tissue CD163 and CD206 levels were higher in recurrent CRSwNP in comparison with primary cases and HCs, and had a positive correlation with TIM-3 levels. TIM-3 overexpression promoted M2 polarisation and enhanced TGF-β1 and IL-10 secretion.
Conclusions. TIM-3 expression was enhanced in patients with CRSwNP, especially in those undergoing revision surgeries. TIM-3 may be a novel biomarker for recalcitrant CRSwNP. TIM-3-driven M2 polarisation might be involved in the mechanisms of recurrent CRSwNP.
Introduction
Chronic rhinosinusitis (CRS) is a complex inflammatory condition of the nose and paranasal sinuses 1. Currently, CRS can be phenotypically divided into CRS with nasal polyps (CRSwNP) or without nasal polyps (CRSsNP) 2. It is well established that patients with CRSwNP have more complex tissue heterogeneity, poorer disease control, and an increased risk of postoperative recurrence 3,4. Previous studies showed that despite nasal endoscopic surgery plus standard postoperative medical therapy, a large proportion of patients still suffer from recurrences 5. Mechanically, high tissue heterogeneity and a complicated immune microenvironment caused by immune cell infiltration and their interactions are the major pathogenetic factors, but the underlying causalities have not been fully elucidated 6,7. Recently, there has been increasing research interest in the pathological mechanisms of CRSwNP, and specifically the role of abnormally activated macrophages 8. Activated macrophages can be classified into classically activated or inflammatory (M1) and alternatively activated or anti-inflammatory (M2). Key biomarkers distinguishing M1 and M2 are primarily NOS2 and CD86 for the former, and CD163 and CD206 for the latter. M1 macrophages contribute to tissue injury and hinder regeneration and wound healing by inducing the generation of reactive oxygen species (ROS). Conversely, M2 macrophages facilitate tissue repair and wound healing by eliminating debris and apoptotic cells, in addition to exhibiting pro-angiogenic and pro-fibrotic properties 9. Polarised macrophages are known to secrete certain cytokines that induce transforming growth factor-beta 1 (TGF-β1) and interleukin 10 (IL-10), which have been shown to negatively impact prognosis and promote disease recurrence 10.
T cell immunoglobulin domain and mucin domain-3 (TIM-3) is an immunomodulatory protein that exhibits broad expression on various immune cells, including T cells and macrophages 11. Accumulating evidence suggests that TIM-3 activates innate immune cells and exhibits proinflammatory effects, which are closely involved in both inflammatory and autoimmune diseases 12. Corredera et al. 13 observed an increase in TIM-3-positive mast cells within the epithelial cell region, which was associated with worsening of postoperative endoscopic findings in CRSwNP patients with comorbid asthma. Furthermore, newly published studies reported that TIM-3 can affect the functions of macrophages and promote reprogramming, which contribute to the immunopathogenesis of pulmonary fibrosis and experimental asthma 12,14. Given the diverse biological function, the polarisation of macrophages driven by TIM-3 is considered to be associated with the initiation and progression of airway inflammation 15. Despite the abundance of research on CRSwNP, there has been no comprehensive investigation into the relationship between TIM-3 and macrophage polarisation in the pathogenesis of this condition. Therefore, it would be interesting to explore the correlations between TIM-3 and macrophage polarisation and their potential impact on CRSwNP.
In this study, we evaluated the expression of TIM-3 in patients with CRSwNP, with a specific focus on those who experienced postoperative recurrence and received revision surgery. Furthermore, we investigated the regulatory effects of TIM-3 on macrophage polarisation. Additionally, we conducted in vitro experiments to explore the role of TIM-3-driven macrophage polarisation in the development and recurrence of CRSwNP.
Materials and methods
Study population and setting
A total of 56 CRSwNP patients were recruited from Changde Hospital (the First People’s Hospital of Changde City) between May 2022 and July 2022, including 28 primary and 28 recurrent CRSwNP. The diagnosis of CRSwNP was established according to the EPOS 2020 criteria 16. We excluded patients with: (1) age < 18 years; (2) co-existing fungal sinusitis, posterior nasal polyp, sinus cyst, and acute respiratory infection; (3) other inflammatory, autoimmune, and immunodeficiency diseases; (4) history of treatment with antibiotics, steroid hormones, antihistamines, and leukotriene receptor antagonists within 4 weeks. Recurrent CRSwNP was confirmed by endoscopic and CT evidence when clinical symptoms relapsed after primary surgery despite the implementation of a rescue regimen involving antibiotics and oral steroids 17. In addition, 28 patients who underwent surgical treatment for nasal bone fracture or simple septal deviation were enrolled as a healthy control (HC) group.
Serum samples were collected from all subjects, and nasal polyps and inferior turbinate specimens were harvested from CRSwNP patients and HCs, respectively. The following data were collected: age, gender, body mass index (BMI), smoking, drinking, co-existing diseases, blood eosinophil levels, Lund-Mackay score, and Lund-Kennedy score.
Enzyme-linked immunosorbent assay (ELISA)
Peripheral blood was collected using a 5 mL vacuum vein blood tube and kept at room temperature for 1 hour. Subsequently, samples were centrifuged at 2000 x g for 10 min at 4°C, and the supernatant was carefully aspirated into a 15 mL centrifuge tube. The tube was then subjected to a second centrifugation at 3000 x g for 3 min. Finally, the resulting supernatant was divided into several aliquots and promptly stored at -80°C for further analysis. The stored serum samples were thawed at room temperature and the levels of soluble TIM-3 were detected using a commercial ELISA kit (Multiscience, China) referring to the commercial instructions. The cell supernatant was harvested and centrifuged at 3000 x g for 10 min, and then the soluble TNF-α, IL-1β, TGF-β1, and IL-10 levels were measured in the cell supernatant by ELISA (Multiscience, China). The experiment result was read at 450 nm using an enzyme immunoassay plate reader with wavelength correction set to 540 nm.
Immunofluorescence staining
Immunofluorescence staining was conducted as described previously 18. In brief, paraffin sections obtained from patients were subjected to deparaffinisation and hydration. Antigen retrieval was performed for 30 min, followed by blocking of nonspecific antigens. The sections were then incubated overnight at 4°C with primary antibodies against human TIM-3, NOS2, CD86, CD163, and CD206 (CST, USA). After washing with phosphate buffered saline solution, sections were incubated with Alexa Fluor 549 secondary antibody (CST, USA) in the dark for 1 hour. Nuclei were counterstained with DAPI for 12 min to enable visualisation. For macrophages, cells were fixed and incubated overnight with antibodies against TIM-3, NOS2, CD86, CD163, and CD206 (CST, USA), followed by incubation with Alexa Fluor 549 secondary antibody (CST, USA) and DAPI staining. All results were visualised using fluorescence microscopy. Representative images were provided for each group, and the number of positive cells was quantified in high-powered fields of view.
Quantitative RT-PCR
Total RNA was isolated from tissues and cells with Trizol reagent (Invitrogen, USA). Complementary DNA (cDNA) was synthesised using reverse transcriptase (Invitrogen, USA). mRNA expression was quantified using an ABI PRISM 7500 detection system (Bio-Rad, USA) and a SYBR Green qPCR kit (Invitrogen, USA). The primer sequences for the target genes are provided in Table S1. Relative mRNA expression was determined using comparative CT values (2 -∆∆CT), and GAPDH was used as a control.
Western blotting
Collected tissues and cells were manually harvested and homogenised. Subsequently, the tissue and cell suspension were lysed in RIPA lysis buffer containing protease inhibitors to extract total protein. Equal amounts of protein extracts were separated by SDS-PAGE gel electrophoresis and transferred onto PVDF membranes (Millipore, USA). The membranes were blocked with 3% BSA for 1.5 hour at room temperature and then incubated with primary antibodies against TIM-3, NOS2, CD86, CD163, CD206, and GAPDH (CST, USA) overnight. The following day, the membranes were incubated with anti-rabbit horseradish peroxidase (HRP)-conjugated secondary antibody (Abcam, USA) for 1.5 hour at room temperature. The protein bands were visualised using an ECL Ultrasensitive luminol substrate, and their intensities were quantified using an imaging system. The relative expression level of the target protein was determined after normalisation to GAPDH.
Peripheral blood macrophage separation, culture, and transfection
Human peripheral blood macrophage was separated as previously described 19. Briefly, peripheral blood specimens were collected from HCs, and peripheral blood mononuclear cells (PBMC) were harvested after gradient centrifugation. The PBMCs were processed to sort out monocytes using anti-CD14 magnetic beads (Miltenyi Biotec, Germany). Monocytes were isolated and sorted and then cultured in RPMI-1640 medium (Peiyuan, China) supplemented with 10% fetal bovine serum (Gibco, USA). To induce macrophage differentiation, M-CSF (Prospec, UK) was added at a concentration of 100 ng/ml, and the cells were incubated for 5 days at 37°C and 5% CO2. The resulting PBMC-derived macrophages were collected and further cultured. For transient transfection, the macrophages were transfected with a TIM-3 expression plasmid using FuGENE® 6 (FuGENE, USA). The treated cells and supernatants were harvested for subsequent experiments.
Statistical analysis
Categorical variables were presented as percentages and compared using the chi-square test. Numeric variables were reported as median and interquartile ranges and compared using the Kruskal-Wallis H test across the three groups. Associations between TIM-3 levels, macrophage markers, and clinical variables were examined by correlation analysis. All statistical analyses were done using SPSS 25.0 software (IBM, USA). A p < 0.05 was regarded as statistically significant.
Results
Comparisons of clinical variables
The characteristics of all subjects among HC, primary, and recurrent CRSwNP groups are listed in Table I. The blood eosinophil levels were markedly elevated in the recurrent CRSwNP compared to the HC and primary groups (p < 0.05). Moreover, the rates of allergic rhinitis and asthma were higher in the recurrent CRSwNP group in comparison with the primary CRSwNP group (p < 0.05). No significant differences were found in other variables among the three groups (p > 0.05).
Elevated TIM-3 in CRSwNP is associated with postoperative recurrence
As presented in Figure 1A, serum TIM-3 concentrations were increased in the CRSwNP group in comparison with the HC group, especially in cases of recurrent CRSwNP. Both RT-PCR and western blot results in Figure 1B-D revealed that TIM-3 expression was enhanced in the tissues of patients with recurrent CRSwNP compared to primary CRSwNP patients and HCs (p < 0.05). The immunofluorescence images in Figure 1E indicated that TIM-3 was overexpressed in the mucosal and submucosal regions of CRSwNP patients compared to HCs, and the number of TIM-3+ cells was greater in the recurrent CRSwNP group than in the primary CRSwNP and HC groups (p < 0.05). Furthermore, Figure 2 shows that TIM-3 expression was significantly higher in the tissue samples during the second recurrence compared to the first recurrence and initial surgery, suggesting that multiple recurrences were associated with a gradual increase in TIM-3 levels.
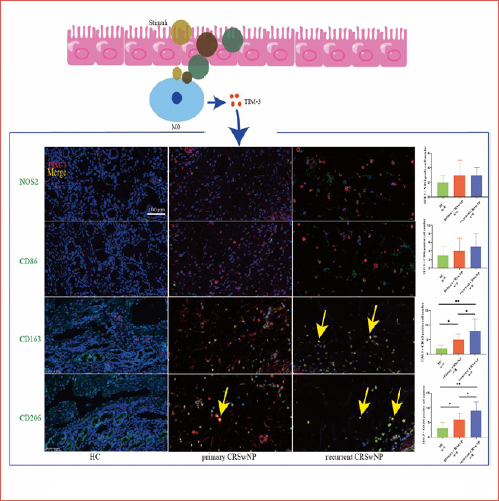
TIM-3 driven macrophage M2 polarisation is associated to CRSwNP recurrence
As macrophages are essential in the pathomechanism of CRSwNP, we evaluated the expressions of macrophage markers in the three groups. In Figure 3, the expression levels of CD86, CD163, and CD206 were found to be higher in the tissues of CRSwNP patients compared to HCs. The elevated CD163 and CD206 levels were particularly significant in cases of recurrent CRSwNP. Furthermore, there was a positive correlation between the mRNA levels of CD163 and CD206 in tissues and the levels of TIM-3. Multiplexed immunofluorescence showed that the co-expression of TIM-3, CD163, and CD206 was higher in the CRSwNP group, particularly in recurrent cases, and most TIM-3 positive cells were co-stained with CD163 and CD206 (Fig. 4). These findings indicate that M2 polarisation is prevalent in the histopathology of CRSwNP, and TIM-3-mediated M2 polarisation may be involved in the mechanisms of recurrence.
Overexpression of TIM-3 aggravates M2 polarisation facilitating CRSwNP recurrence
To further explore the impact of TIM-3 on M2 polarisation, we used plasmids to overexpress TIM-3 in macrophages. Immunofluorescence images, RT-PCR, and western blot results suggested that TIM-3 overexpression profoundly increased the levels of CD163 and CD206, but these influences on CD80 and CD86 were inappreciable. ELISA results demonstrated a marked increase in the protein levels of both TGF-β1 and IL-10 in the cell supernatant from cells treated with TIM-3 plasmids (Fig. 5). Taken together, these data suggest that TIM-3 may play a role in promoting M2 polarisation and the production of TGF-β1 and IL-10, which may contribute to the recurrence of CRSwNP.
Discussion
The mechanisms responsible for the recurrence of CRSwNP are not yet fully understood. Our study provides initial evidence that both circulating and tissue levels of TIM-3 are elevated in CRSwNP patients and are closely linked to its postoperative recurrence. Furthermore, we discovered that TIM-3 can induce macrophage M2 polarisation and increase production of TGF-β1 and IL-10, suggesting that TIM-3 might serve as a potential contributor to the mechanisms underlying recurrence.
Macrophages are crucial members of innate immune cells with high plasticity and heterogeneity, and have important effects in tumour immunity and inflammation response 20. It has been reported that macrophages were recruited to release various mediators in tissue after inflammatory injury and accelerate tissue repairment and remodeling, which contributed to the histopathology of chronic inflammatory disorders 21. Macrophages have also been implicated in the pathogenesis of CRSwNP and are associated with severity of the disease 19. However, the potential roles of macrophage polarisation in recurrent CRSwNP and underlying regulatory mechanisms remain to be discovered. In this study, we found that M2 markers were significantly enhanced in CRSwNP, especially in recurrent disease, suggesting that M2 polarisation predominated in the recurrent pathology. Therefore, exploring the underlying mechanisms of M2 polarisation is pivotal to further understand the mechanisms underlying recurrence of CRSwNP and developing a precise treatment.
TIM-3 is well known as an important molecule that is primarily expressed on CD4+ T cells 11. Recently, accumulating evidence has shown that TIM-3 is also commonly observed on innate immune cells, including macrophages and dendritic cells, and exhibits a role in proinflammatory cytokine production 22. Evidence suggests that TIM-3 regulates macrophage activation according to their function, with M2 macrophages overexpressing TIM-3, whereas M1 macrophages exhibit lower TIM-3 expression 23. Abnormally expressed TIM-3 was found to be essential in the immune microenvironment of several inflammatory and allergic diseases 14. In our study, we found that levels of TIM-3 are increased in the serum and nasal polyps of patients with CRSwNP. Additionally, we found a correlation between heightened TIM-3 expression and the risk of recurrence. Interestingly, we observed that as the number of relapses increased, TIM-3 levels also increased in tissue samples. We also noted that TIM-3 was selectively expressed on CD163+ and CD206+ macrophages and that the amount of co-expressed M2 cells was significantly higher in recurrent cases. Based on our findings, we suspect that excessive expression of TIM-3 in macrophages may be involved in the mechanisms of recurrent CRSwNP.
To examine whether TIM-3 can drive M2 polarisation and facilitate the recurrence of CRSwNP, we overexpressed TIM-3 in PBMC-derived macrophages. We found that the upregulation of TIM-3 could profoundly intensify the expression of CD163 and CD206 and promote the secretion of TGF-β1 and IL-10. These results highlight that TIM-3 is likely involved in regulating the functions of macrophages, and elevated TIM-3 levels could promote M2 polarisation and secretion of cytokines, which might mediate the recurrence of CRSwNP. Furthermore, M2 macrophages consist of various subpopulations. For instance, the M2a subpopulation can be induced by IL-4 and IL-13, contributing to tissue remodeling through the production of cytokines such as CCL18, CCL22, and CCL24. This, in turn, promotes eosinophilia and airway inflammation.
On the other hand, the M2c subpopulation demonstrates potent anti-inflammatory activity by releasing significant amounts of IL-10 and TGF-β, particularly in response to apoptotic cells 9. It has been reported that recurrent CRSwNP is usually characterised by tissue remodelling, including epithelial-mesenchymal transition (EMT) and eosinophilia 6. Previous studies highlighted that chemokines and cytokines, such as CCL-24 and IL-10, can recruit eosinophils and facilitate their infiltration into tissues24. Additionally, TGF-β1 was observed to be essential for aggravating the EMT in nasal polyps formation, contributing to poor prognosis and relapse 25. Herein, we observed that TIM-3 could activate the secretions of TGF-β1 and IL-10 in PBMC-derived macrophages, and accumulated levels of them might exacerbate the risk of postoperative recurrence of CRSwNP by accelerating the tissue eosinophil infiltration and EMT. Therefore, we have reasons to believe that TIM-3-driven M2 polarisation might facilitate the mechanisms underlying recurrent CRSwNP, and TIM-3 may be a potential biomarker to predict postoperative recurrence. Moreover, it is crucial to highlight the significant role of IL-13/IL-4 in the M2 polarisation network, as it profoundly influences the pathogenesis and treatment of CRSwNP.
We recognise that there are several potential limitations of the present study. First, the study was performed in a single medical centre, and the participants were recruited from a similar region and with the same ethnicity, which may limit the external validity of this work. Second, the number of serum and tissue samples utilised was relatively limited which could lead to selection bias. Thirdly, we only performed a comparative analysis of TIM-3 expression in primary and recurrent CRSwNP patients, along with analysing the changes in TIM-3 in a limited number of cases before and after recurrence. Therefore, the conclusions should not be overly enthusiastic. Finally, we did not perform animal experiments to further confirm the conclusions derived from clinical samples and in vitro experiments.
Conclusions
To conclude, our findings revealed that TIM-3 is enhanced in CRSwNP patients and positively associated with expression of macrophage M2 markers, especially in those undergoing revised surgeries. TIM-3 appears to be a novel biomarker with potential in predicting postoperative recurrence and as a therapeutic target in CRSwNP. TIM-3-driven macrophage M2 polarisation might play a significant role in the mechanisms involved in recurrence of CRSwNP. Further large-sample, multicentre studies are needed to confirm our results.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
TJ: contributed to manuscript writing; TY, LJ: contributed to conducting the experiments, and ZT: contributed to the design of experiments and manuscript review.
Ethical consideration
This study was approved by the Institutional Ethics Committee of Changde Hospital (the First People’s Hospital of Changde City) (No. YX-2023-067-01).
The research was conducted ethically, with all study procedures being performed following the requirements of the World Medical Association’s Declaration of Helsinki.
Written informed consent was obtained from each participant/patient for study participation and data publication.
History
Received: August 10, 2023
Accepted: January 31, 2024
Figures and tables
Figure 1. The expression of TIM-3 in serum and tissue samples among the three groups. (A) Circulating TIM-3 levels were enhanced in recurrent CRSwNP compared to primary CRSwNP and HCs; (B-D) Tissue TIM-3 was enhanced in CRSwNP patients, especially in the recurrent group. (E) Tissue immunofluorescence staining of TIM-3 among the three groups.
Figure 2. Immunofluorescence images depicting TIM-3 in various tissue samples obtained from a CRSwNP patient who experienced two postoperative recurrences.
Figure 3. Comparisons of M1 and M2 marker expression in the three groups. (A-D) CD86, CD163, and CD206 were enhanced in the CRSwNP group, and CD163 and CD206 were enhanced in the recurrent group compared to the primary group; (E-H) Tissue TIM-3 mRNA levels correlated with CD163 and CD206 levels; (I-J) The tissue protein levels of CD163 and CD206 were up-regulated in the recurrent CRSwNP group compared to the primary CRSwNP and HC groups.
Figure 4. Multiple immunofluorescence staining of TIM-3 and macrophage markers among the three groups.
Figure 5. The influence of TIM-3 overexpression on macrophage polarisation. (A-B) Cell immunofluorescence staining revealed stronger fluorescence intensity in the OE-TIM-3 group compared to the HC group; (C) RT-PCR revealed that the CD86, CD163, and CD206 were augmented in the OE-TIM-3 group when compared to the HC group; (D-E) WB showed that NOS2, CD163, and CD206 were enhanced in the OE-TIM-3 group in comparison to the HC group; (E) IL-1β,TGF-β1, and IL-10 were increased in the cell supernatants collected from the OE-TIM-3 group in comparison with the HC group.
| Variables | HC | Primary CRSwNP | Recurrent CRSwNP | P |
|---|---|---|---|---|
| (n = 28) | (n = 28) | (n = 28) | ||
| Age, year | 42 (37, 51) | 44 (39, 52) | 43 (37, 53) | 0.563 |
| Male/female | 17/11 | 16/12 | 16/12 | |
| BMI, kg/m2 | 23.8 (21.9, 25.6) | 24.3 (22.1, 25.9) | 24.1 (22.3, 26.2) | 0.318 |
| Smoking, (n, %) | 8 (28.6) | 9 (32.1) | 7(25) | 0.952 |
| Drinking, (n, %) | 4 (14.3) | 5 (17.9) | 5 (17.9) | 0.918 |
| Allergic rhinitis, (n, %) | 0 (0) | 4 (14.3) | 9 (32.1) | 0.004 |
| Asthma, (n, %) | 0 (0) | 3 (10.7) | 7(25) | 0.015 |
| Blood eosinophil count (106/L) | 152.3 (102.3, 245.7) | 247.1 (163.8, 317.9) | 332.8 (277.9, 378.9) | < 0.001 |
| Blood eosinophil percentage | 2.9 (2.1, 4.2) | 3.6 (2.8, 5.3) | 4.9 (3.8, 6.1) | < 0.001 |
| Lund-Mackay score | - | 13 (9, 15) | 14 (10, 16) | 0.436 |
| Lund-Kennedy score | - | 7 (5, 9) | 8 (5, 9) | 0.812 |
| Number of previous surgeries | ||||
| 1 | - | 0 (0) | 20 (71.4) | < 0.001 |
| 2 | - | 0 (0) | 8 (28.6) | 0.004 |
| HC: healthy control; CRSwNP: chronic rhinosinusitis with nasal polyps; BMI: body mass index. | ||||
| Gene | Forward primer | Reverse primer |
|---|---|---|
| TIM-3 | ATGTCCGTCGATGAGGGAGTGGGT | TCCTGCTCCCCGACAATGCACACA |
| NOS2 | GCTACAGCTTGAGTGCTTTCCCCA | AACAGGGGTGCCTTTGCCTGACCCT |
| CD86 | ACAGGGACTAGCACAGACACACGGA | AGCACCATCTTCAACCTCAGCCT |
| CD163 | GAGCAAACTCAGAATGGTGCT | AGGTGCTGCCATATAAGCCTATGT |
| CD206 | TGCGTCTTAGTTCCGCCCTCCTGT | AGGTCAGAGATCCCCTGCCTCA |
| GAPDH | TTGCAGTCGTATGGGGGCAGGGTAGCT | AGGGACCTCCTGTTTCTGGGGACT |
References
- Sedaghat A, Fokkens W, Lund V. Consensus criteria for chronic rhinosinusitis disease control: an international Delphi Study. Rhinology. 2023;61:519-530. doi:https://doi.org/10.4193/Rhin23.335
- Fokkens W, Viskens A, Backer V. EPOS/EUFOREA update on indication and evaluation of Biologics in Chronic Rhinosinusitis with Nasal Polyps 2023. Rhinology. 2023;61:194-202. doi:https://doi.org/10.4193/Rhin22.489
- Xie S, Zhang C, Xie Z. Serum metabolomics identifies uric acid as a possible novel biomarker for predicting recurrence of chronic rhinosinusitis with nasal polyps. Rhinology. 2023;61:541-551. doi:https://doi.org/10.4193/Rhin23.236
- Xu X, Seet J, Yap Q. Latent class analysis of structured histopathology in prognosticating surgical outcomes of chronic rhinosinusitis with nasal polyps in Singapore. Rhinology. 2023;61:358-367. doi:https://doi.org/10.4193/Rhin22.455
- Chen W, Bai Y, Kong W. Predictive significance of Charcot-Leyden crystal structures for nasal polyp recurrence. Clin Transl Allergy. 2022;12. doi:https://doi.org/10.1002/clt2.12212
- Wu P, Chiu C, Huang Y. Tissue eosinophilia and computed tomography features in paediatric chronic rhinosinusitis with nasal polyps requiring revision surgery. Rhinology. 2023;61:348-357. doi:https://doi.org/10.4193/Rhin22.435
- Kim D, Han J, Kim G. Clinical predictors of polyps recurring in patients with chronic rhinosinusitis and nasal polyps: a systematic review and meta-analysis. Rhinology. 2023;61:482-497. doi:https://doi.org/10.4193/Rhin23.136
- Chen J, Chen S, Gong G. Inhibition of IL-4/STAT6/IRF4 signaling reduces the epithelial-mesenchymal transition in eosinophilic chronic rhinosinusitis with nasal polyps. Int Immunopharmacol. 2023;121. doi:https://doi.org/10.1016/j.intimp.2023.110554
- Shapouri-Moghaddam A, Mohammadian S, Vazini H. Macrophage plasticity, polarization, and function in health and disease. J Cell Physiol. 2018;233:6425-6440. doi:https://doi.org/10.1002/jcp.26429
- Wang Z, Yao Y, Wang N. Deficiency in interleukin-10 production by M2 macrophages in eosinophilic chronic rhinosinusitis with nasal polyps. Int Forum Allergy Rhinol. 2018;8:1323-1333. doi:https://doi.org/10.1002/alr.22218
- Ueland T, Heggelund L, Lind A. Elevated plasma sTIM-3 levels in patients with severe COVID-19. J Allergy Clin Immunol. 2021;147:92-98. doi:https://doi.org/10.1016/j.jaci.2020.09.007
- Wang Y, Kuai Q, Gao F. Overexpression of TIM-3 in macrophages aggravates pathogenesis of pulmonary fibrosis in mice. Am J Respir Cell Mol Biol. 2019;61:727-736. doi:https://doi.org/10.1165/rcmb.2019-0070OC
- Corredera E, Phong B, Moore J. TIM-3-expressing mast cells are present in chronic rhinosinusitis with nasal polyps. Otolaryngol Head Neck Surg. 2018;159:581-586. doi:https://doi.org/10.1177/0194599818774560
- Boehne C, Behrendt A, Meyer-Bahlburg A. Tim-3 is dispensable for allergic inflammation and respiratory tolerance in experimental asthma. PLoS One. 2021;16. doi:https://doi.org/10.1371/journal.pone.0249605
- Athari S. Targeting cell signaling in allergic asthma. Signal Transduct Target Ther. 2019;4. doi:https://doi.org/10.1038/s41392-019-0079-0
- Fokkens W, Lund V, Hopkins C. European Position Paper on rhinosinusitis and nasal polyps 2020. Rhinology. 2020;58:1-464. doi:https://doi.org/10.4193/Rhin20.600
- Sella G, Tamashiro E, Sella J. Asthma is the dominant factor for recurrence in chronic rhinosinusitis. J Allergy Clin Immunol Pract. 2020;8:302-309. doi:https://doi.org/10.1016/j.jaip.2019.08.007
- Zhang J, Cheng S, Xie S. Significance of leukocyte-specific transcript 1 levels in nasal mucosal tissue to predict recurrence of nasal polyps. Braz J Otorhinolaryngol. 2023;89:321-328. doi:https://doi.org/10.1016/j.bjorl.2022.11.004
- Wang W, Xu Y, Wang L. Single-cell profiling identifies mechanisms of inflammatory heterogeneity in chronic rhinosinusitis. Nat Immunol. 2022;23:1484-1494. doi:https://doi.org/10.1038/s41590-022-01312-0
- Preteroti M, Wilson E, Eidelman D. Modulation of pulmonary immune function by inhaled cannabis products and consequences for lung disease. Respir Res. 2023;24. doi:https://doi.org/10.1186/s12931-023-02399-1
- Huang Z, Shen S, Han X. Macrophage DCLK1 promotes atherosclerosis via binding to IKKβ and inducing inflammatory responses. EMBO Mol Med. Published online 2023. doi:https://doi.org/10.15252/emmm.202217198
- Li Z, Wang Y, Zheng K. Tim-3 blockade enhances the clearance of Chlamydia psittaci in the lung by promoting a cell-mediated immune response. Int Immunopharmacol. 2023;116. doi:https://doi.org/10.1016/j.intimp.2023.109780
- Ocaña-Guzman R, Ramon-Luing L, Vazquez-Bolaños L. Tim-3 is differentially expressed during cell activation and interacts with the LSP-1 protein in human macrophages. J Immunol Res. 2023;2023. doi:https://doi.org/10.1155/2023/3577334
- Zhu Z, Wang W, Zhang X. Nasal fluid cytology and cytokine profiles of eosinophilic and non-eosinophilic chronic rhinosinusitis with nasal polyps. Rhinology. 2020;58:314-322. doi:https://doi.org/10.4193/Rhin19.275
- Jo S, Lee S, Jo H. Eosinophil-derived TGFβ1 controls the new bone formation in chronic rhinosinusitis with nasal polyps. Rhinology. 2023;61:338-347. doi:https://doi.org/10.4193/Rhin22.439
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2024 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 338 times
- PDF downloaded - 146 times



 PDF
PDF
