Reviews
Vol. 44: Issue 4 - August 2024
Endoscopic transnasal approach to remove an intraorbital bullet: systematic review and case report
Abstract
Introduction. Intraorbital foreign bodies (IOFBs) represent a clinical challenge: surgical management can be controversial and different strategies have been proposed. When removal is recommended, depending on the location and nature of the IOFB both external and endoscopic approaches have been proposed, with significantly different surgical corridors to the orbit and different morbidities.
Methods. We performed a literature review of cases of IOFBs that received exclusive endoscopic transnasal surgical treatment to evaluate the role of this surgery in these occurrences. We also present a case of an intraorbital intraconal bullet that was successfully removed using an endoscopic transnasal approach with good outcomes in terms of ocular motility and visual acuity.
Results. A limited number of cases of IOFBs have been treated with an exclusive endoscopic transnasal approach. When in the medial compartment, this approach appears to be safe and effective.
In our case, two months after surgery the patient showed complete recovery with no significant long-term sequelae.
Conclusions. When feasible, an endoscopic transnasal approach for intraorbital foreign bodies represents a valid surgical technique with optimal outcomes and satisfactory recovery.
Introduction
Management of orbital bullets, and more in general bullets of the sino-orbital region, can be found in few reports in the literature 1.
Intraorbital foreign bodies (IOFBs) are described as objects that are inside the orbital space but outside the ocular globe. IOFBs can be found more often after trauma, for example, due to a gunshot or other high-velocity injuries; in some cases, they can show little evidence of their presence 2,3.
IOFBs can be classified according to their material: inorganic foreign bodies are generally associated with visual loss or orbital complications from direct trauma, while organic IOFBs are related to a higher incidence of orbital and intracranial infections 4.
Injuries related to IOFBs can often lead to serious consequences, but in some cases proper management can avert major complications and provide good long-term prognosis 4.
Different approaches have been used to remove IOFBs including bullets 5. A conventional approach can be performed with open techniques, such as transconjunctival approaches or other orbitotomy procedures 6; open surgeries are the most common procedures and are performed primarily by ophthalmologists 7.
Nowadays, the evolution of endoscopic techniques allows an effective direct approach to all intraconal compartments (medial, inferior, superior and lateral) with a low risk of damaging orbital structures 8,9.
We report a clinical case of a young male who was injured by gunfire with a bullet that penetrated inside the intraorbital intraconic space and was surgically treated with a transnasal endoscopic approach to remove the foreign body.
We also performed a literature review of cases of IOFBs that underwent an endoscopic transnasal treatment as the only approach to evaluate the role of this surgery in this clinical condition.
Materials and methods
We performed a review of literature using PubMed, Scopus and Web of Science databases using the words [orbit] or [orbital] and [foreign body] and [endoscopic] and [removal]. We retrieved 76 articles and performed a selection according to PRISMA flowchart 10 (Fig. 1). Twelve articles were selected that regarded cases of IOFBs removed with an endoscopic transnasal approach, excluding cases that involved the orbit but had the foreign body located in different sites. We also excluded articles on IOFBs that were treated with surgical approaches other than an endoscopic transnasal procedure and those treated with combined approaches.
Case report
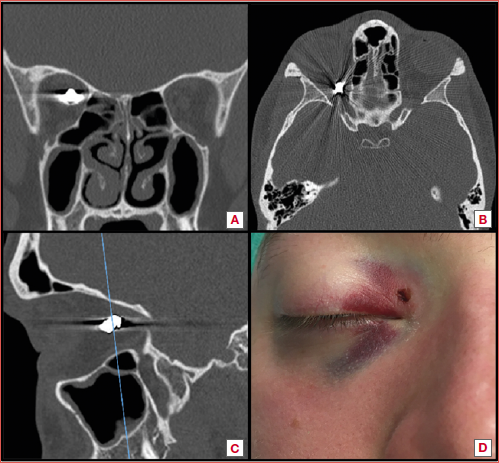
A 22-year-old male came to our attention after he was shot with an air rifle, presenting with a bullet penetrating the medial intraconal space of the right eye. No other traumatic injuries of the maxillo-facial compartment were present (Cover figure). The patient complained of almost complete loss of vision in the right eye.
Pre-operative ophthalmologic evaluation showed limited motility in adduction of the right eye with pain due to the impairment of the right medial rectus muscle (MRM). He also had a right relative afferent pupillary defect and visual acuity of the right eye of 1/10, without any lesion of the ocular bulb.
After providing detailed informed consent, we decided to perform an endoscopic transnasal procedure to remove the foreign body considering its position in relation to the optic nerve (ON).
We used an intra-operative magnetic neuronavigation system (StealthStation, Medtronic) to facilitate localisation of the bullet inside the orbit, since the lack of fixed landmarks can make this operation challenging and prolong surgical time.
We used a transnasal transethmoidal approach to open and partially remove the lamina papyracea. Next we opened the periorbit and located the MRM. After that, using blunt instruments, we proceeded with dissection of the intraconal fat using the operative window between the superior edge of MRM and the superior oblique muscle. During the procedure, we localised the correct surgical area with the help of the navigation system and used intraoperative traditional X-ray scans to establish the position of the foreign body relative to the localisation of a surgical instrument used as a radiopaque landmark (Fig. 2).
No anomalous bleeding occurred, and all functional structures were preserved. Intraoperative findings confirmed the position of the bullet close to the ON. However, there was no surgical trauma to the nerve. The patient was discharged three days after surgery. He did not refer pain or discomfort after the procedure.
We performed an endoscopic control after three weeks, showing good healing in the right nasal fossa. Ocular motility was preserved. Ophthalmological evaluation at 4 days, 15 days, 2 months, and 3 months after surgery revealed significant improvement in the visual field test (Fig. 3).
Results
According to our literature review, the presence of IOFBs is quite a rare finding in common ENT and neurosurgical practice. Management can be conservative or surgical. When surgery is performed to remove IOFBs, different approaches can be chosen: endoscopic, open, or a combination of both techniques.
In line with the purpose of our systematic review, only reports of patients treated with an exclusive endoscopic approach (12 articles and 18 patients) were selected and the results are summarised in Table I.
Patients were more often male (M:F = 7:4; for 7 patients we could not retrieve the gender). Mean age was 30.6 years. Foreign bodies were of different types: bullets, wooden sticks, metallic fragments, glass foreign bodies, pencils, and other blunt objects; even a dental implant was recorded.
At the time of first clinical evaluation, patients presented different features, ranging from total absence of any symptom to complete loss of vision.
After endoscopic transnasal surgery, the outcome was generally good, with recovery (total or complete) in 9 reports. In one patient binocular diplopia persisted after surgery and in another one visual acuity remained compromised. None of the reports showed worsening of clinical conditions after an endoscopic transnasal approach.
Discussion
Treatment of orbital lesions can be controversial considering different surgical options according to the type of lesion and its location inside the orbital space 11. Considering IOFBs, diagnosis and management require special attention. IOFBs are reported to occur in one out of six orbital injuries 12. According to the indications for trauma surgeons, in case of retained bullets, situations that indicate the need for removal are: bullets in joints or the globe of the eye, associated cerebro-spinal fluid leak, nerve impingement, bullets within a vessel lumen, lead poisoning, bullets seen or clinically palpated and medico-legal purposes 13.
Clinically, patients need ophthalmological evaluation to assess visual impairment checking visual acuity and visual fields, as well as other complications related to the orbital trauma (e.g., motility impairment of extrinsic eye muscles) 14.
Damage to the ON can occur with primary or secondary mechanisms 15 and visual function might worsen with direct or indirect mechanisms 16. Therefore, dealing with an intraorbital bullet, surgery can be difficult to perform without risks for visual function or ocular motility. Some authors report that IOFBs can be well-tolerated for up to 68 years, with minimal adverse prognosis 17. However, the retaining of an IOFB can cause complications such as chronic orbital inflammation, osteomyelitis, thrombotic vasculitis, or infections 5. According to other authors, both organic and inorganic foreign bodies should be removed to avoid late complications from inert and non-inert materials 2,18. The position inside the orbital space must be considered for management, since foreign bodies located posteriorly have been reported to have an increased risk of ocular motility impairment when surgically removed 17. However, the endoscopic transnasal approach offers advantages compared to open approaches as it allows a direct corridor to the surgical field.
Other evidence shows that IOFBs can present spontaneous anterior migration that can lead to mechanical and inflammatory complications, which then represent a clear surgical indication for removal 19. For these reasons and considering our experience, it is important to remove bullets or other foreign bodies as soon as possible when surgery is feasible, especially when a minimally invasive approach can be performed.
For radiological evaluation it is fundamental to use a non-enhanced computed tomography (CT) as the initial imaging of choice as it is rapid, generally easily available, easy to access, and has a high sensitivity for acute haemorrhagic lesions 20. Magnetic resonance imaging (MRI) should be reserved for detection of lesions that may remain unclear after initial CT scan 21, but if a magnetic component is suspected to be included in the bullet, MRI should be avoided.
In case of gunshot injuries with intraorbital bullets, patients should be managed as soon as the patient is clinically stable after trauma to decide on the proper approach to prevent further complications 1, with impairment of visual function and severe intraorbital inflammation justifying surgical treatment 7. In our case, we decided to operate as the patient presented significant visual impairment with compromised integrity of the ON according to CT.
Different surgical techniques have been described to approach IOFBs. Open conventional approaches include orbitotomy, transconjunctival or transseptal entries 17, or a craniotomic approach when a concomitant intracranial injury is suspected 22. These surgical procedures are not devoid of disadvantages, as they present considerable sequelae and post-surgical scarring.
An endoscopic transnasal approach to the orbital compartment is a less invasive, safe procedure that gives direct visualisation. Exclusive endoscopic removals of a bullet from the orbit have been reported in the literature with good results 5,24-26.
According to the literature, a limited number of cases of IOFBs have been treated with an exclusive endoscopic transnasal approach (Tab. I) 3,5,25-34. The localisation of the IOFB in these cases was usually medial to the ON and treatment was performed without significant complications.
The endoscopic transnasal transethmoidal approach is feasible for lesions including foreign bodies near the medial wall of the orbit and those located in the medial intraconal compartment, medially to the optic nerve 9,25,35.
It is a safe, minimally invasive approach that allows the removal of the orbital foreign body and at the same time exposes and preserves the extraconal structures of the medial orbit, such as the inferior and medial rectus muscles, with minimal damage to surrounding tissues; it also prevents postsurgical external scarring and reduces bleeding complications 36.
The implementation of new technologies in endoscopic transnasal surgery gives great advantages to surgeons. The use of a navigation system, borrowed from neurosurgical experience, facilitates the localisation of the surgical target, based on the pre-operative imaging, with advantages on surgical times and manipulation 37. After opening the periorbit, navigation can be less precise as spaces change compared to pre-operative CT or MRI. In this condition, endoscopic transnasal approaches to the orbit can benefit from the use of intraoperative X-rays and/or ultrasonography to localise the lesion or foreign body and to identify the best surgical corridor for each procedure, effectively helping the surgeon and potentially reducing operative complications 38.
Conclusions
Transnasal endoscopic surgery is currently performed for a significant number of conditions in the sinonasal, orbital, and skull base regions. It is widely considered a safe surgical technique to access the medial intraconal and posterior orbital spaces with little morbidity for the patient. In selected cases, endoscopic surgery can provide an excellent approach to foreign bodies of the orbit including bullets from gunshots.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
GS, AG: investigation, methodology, resources, writing – original draft and editing; MZ, PF, GA, FA, DM: editing, reviewing; EP: conceptualisation, methodology, supervision, writing – reviewing and editing.
Ethical consideration
The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
Written informed consent was obtained from the patient for data publication.
History
Received: December 20, 2023
Accepted: February 5, 2024
Published online: May 2, 2024
Figures and tables
Figure 1. PRISMA 2020 flow diagram for endoscopic transnasal approach for intraorbital foreign bodies.
Figure 2. A,B) Intra-operative X-rays: with the help of a metallic instrument, the bullet was more easily located during our surgical procedure; C) intraoperative endoscopic view of the bullet inside intraconal space. MRM: medial rectus muscle, SOM: superior oblique muscle, ICF: intraconal fat, white star: bullet.
Figure 3. Visual field test: four days after trauma (A), 15 days after surgery (B), 2 months after surgery (C), and 3 months after surgery (D).
| Author(s) | Age | Gender | Type of IOFB | Clinical presentation | Outcome |
|---|---|---|---|---|---|
| Khan-Lim et al., 1999 27 | 40 | M | Blunt object | Decreased visual acuity, limitation in right abduction and depression | Recovery of vision acuity |
| Khyani et al., 2008 28 | 18 | F | Bullet | NR | Good recovery |
| Koo et al., 2008 34 | 24 | M | Ballpoint pen (fragment) | Reduced visual acuity, mild relative afferent pupillary defect and visual field defect in the inferonasal aspect on the left side | Visual acuity improvement |
| Teh et al., 2016 26 | 40 | M | Metal shard | Loss of vision, right relative afferent defect | Reverse relative afferent pupillary defect gradually resolved after 2 endoscopic surgeries |
| Escobar Montatixe et al., 2016 25 | 41 | F | Glass FB | Recurrent left orbital edema and erythema (surgery performed 5y after injury) | Good recovery |
| Wen et al., 2017 29* | 11 (median) | NR | Bullet/explosion fragment/tree branch/iron bar/pencil | 4 patients with pre-operative vision loss | NR |
| Promsopa et al., 2019 5 | 26 | F | Metallic FB | Asymptomatic | Good recovery |
| Levin et al., 2019 30 | 45 | M | Metallic FB | Diplopia secondary to complete third, fourth and sixth nerve palsies | Persistent binocular diplopia |
| Zhao et al., 2019 3 | 36 | M | Bullet | Direct light reflex disappeared, dysfunction in adduction and abduction, decreased visual acuity | Visual acuity and extraocular motility improvement |
| Bocchialini et al., 2020 31 | 55 | F | Dental implant | Limited eye muscles movement, scotoma | Good recovery |
| Sasindran et al., 2022 32 | 12 | M | Wooden stick | Oedema and restriction of eye movements | Complete recovery |
| Hou et al., 2022 33 | 20 | M | Metal bullet | Vision loss | Visual acuity remained compromised |
| M: male; F: female; FB: foreign body; NR: not reported. *: Authors reported 28 cases with 7 out of 28 patients with FB stopping their trajectories in the orbital compartment. | |||||
References
- Viljoen G, Tromp S, Goncalves N, et al. Orbito-cranial gunshot injuries with retained sinonasal bullets. J Maxillofac Oral Surg 2021;20:551-557. https://doi.org/10.1007/s12663-020-01365-4
- Fulcher TP, McNab AA, Sullivan TJ. Clinical features and management of intraorbital foreign bodies. Ophthalmology 2002;109:494-500. https://doi.org/10.1016/S0161-6420(01)00982-4
- Zhao Y, Liu J, Wang Z, et al. Transnasal endoscopic retrieval of a metallic intraorbital intraconal foreign body facilitated by an intraoperative magnetic stick. J Craniofac Surg 2019;30:E603-E605. https://doi.org/10.1097/SCS.0000000000005622
- Callahan AB, Yoon MK. Intraorbital foreign bodies: retrospective chart review and review of literature. Int Ophthalmol Clin 2013;53:157-165. https://doi.org/10.1097/IIO.0b013e3182a12b55
- Promsopa C, Prapaisit U. Removal of intraconal bullet through endoscopic transnasal surgery with image-guided navigation system 8 months after injury: a case report. J Med Case Rep 2019;13:65. https://doi.org/ 10.1186/s13256-019-2007-x
- Griffa A, Viterbo S, Boffano P. Endoscopic-assisted removal of an intraorbital dislocated dental implant: displaced dental implant in the orbit. Clinical Oral Implants Res 2010;5;21:778-780. https://doi.org/10.1111/j.1600-0501.2009.01894.x
- Huang YT, Kung WH, Chang CH, et al. Endoscopy-assisted extraction of orbital and nasal foreign body. Taiwan J Ophthalmol 2021;11:421. https://doi.org/10.4103/tjo.tjo_47_20
- Łysoń T, Sieskiewicz A, Rogowski M, et al. Transnasal endoscopic removal of intraorbital wooden foreign body. J Neurol Surg A Cent Eur Neurosurg 2012;3;74:E100-E103. https://doi.org/10.1055/s-0032-1326942
- Dallan I, Seccia V, Lenzi R, et al. Transnasal approach to the medial intraconal space: anatomic study and clinical considerations. Minim Invasive Neurosurg 2010;53:164-168. https://doi.org/10.1055/s-0030-1263106
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol 2021;134:178-189. https://doi.org/10.1016/j.jclinepi.2021.03.001
- Zoli M, Sollini G, Milanese L, et al. Endoscopic approaches to orbital lesions: case series and systematic literature review. J Neurosurg 2021;134:608-620. https://doi.org/10.3171/2019.10.JNS192138
- Jabang JN, Dampha L, Sanyang B, et al. Management of a large intraorbital wooden foreign body: case report. Surg Neurol Int 2020;20;11:158. https://doi.org/10.25259/SNI_204_2020
- Dienstknecht T, Horst K, Sellei RM, et al. Indications for bullet removal: overview of the literature, and clinical practice guidelines for European trauma surgeons. Eur J Trauma Emerg Surg 2012;38:89-93. https://doi.org/10.1007/s00068-011-0170-x
- Atkins EJ, Newman NJ, Biousse V. Post-traumatic visual loss. Rev Neurol Dis 2008;5:73-81.
- Walsh FB. Pathological-clinical correlations. I. Indirect trauma to the optic nerves and chiasm. II. Certain cerebral involvements associated with defective blood supply. Invest Ophthalmol 1966;5:433-449.
- Karimi S, Arabi A, Ansari I, et al. A systematic literature review on traumatic optic neuropathy. J Ophthalmol 2021;26;2021:1-10. https://doi.org/10.1155/2021/5553885
- Ho VH, Wilson MW, Fleming JC, et al. Retained intraorbital metallic foreign bodies. Ophthalmic Plast Reconstr Surg 2004;20:232-236. https://doi.org/10.1097/01.IOP.0000129014.94384.e6
- Espaillat A. Intraorbital metallic foreign body. Arch Ophthalmol 1998;1;116:824. https://doi.org/10.1001/archopht.116.6.824
- Mendes PD, Fariña EG, De Aguiar GB, et al. Changes in management strategies after spontaneous migration of a retained intraorbital metallic foreign body. J Craniofacial Surg 2010;21:1295-1296. https://doi.org/10.1097/SCS.0b013e3181e2080e
- Bodanapally UK, Sours C, Zhuo J, et al. Imaging of traumatic brain injury. Radiol Clin North Am 2015;53:695-715. https://doi.org/10.1016/j.rcl.2015.02.011
- Currie S, Saleem N, Straiton JA, et al. Imaging assessment of traumatic brain injury. Postgraduate Medical Journal 2016;1;92:41-50. https://doi.org/10.1136/postgradmedj-2014-133211
- Marchioni D, Bertossi D, Soloperto D, et al. Traumatic intraconal foreign body: report of an injury corrected with combined surgical and endoscopic treatment. Operative Neurosurg 2016;12:14-18. https://doi.org/10.1227/NEU.0000000000001150
- Schreckinger M, Orringer D, Thompson BG, et al. Transorbital penetrating injury: case series, review of the literature, and proposed management algorithm: report of 4 cases. J Neurosurg 2011;114:53-61. https://doi.org/10.3171/2010.8.JNS10301
- Feichtinger M, Zemann W, Kärcher H. Removal of a pellet from the left orbital cavity by image-guided endoscopic navigation. Int J Oral Maxillofac Surg 2007;36:358-361. https://doi.org/10.1016/j.ijom.2006.11.008
- Escobar Montatixe D, Villacampa Aubá JM, Sánchez Barrueco Á, et al. Transnasal, transethmoidal endoscopic removal of a foreign body in the medial extraconal orbital space. Case Rep Otolaryngol 2016;2016:1-4. https://doi.org/10.1155/2016/1981456
- Teh D, Mohamad NF, Lim E, et al. Endoscopic transnasal removal of an intraconal foreign body using an image-guided surgical system. Comput Assist Surg 2016;1;21:25-28. https://doi.org/10.3109/24699322.2016.1170884
- Khan-Lim D, Ellis J, Saleh H, et al. Endoscopic transnasal removal of orbital foreign body. Eye (Lond) 1999;13:667-668. https://doi.org/10.1038/eye.1999.181
- Khyani M, Hafeez A, Farooq MU, et al. Endoscopic removal of bullet from orbital apex. J Coll Physicians Surg Pak 2008;18:646-648. https://doi.org/10.2008/JCPSP.646648
- Wen YH, Hou WJ, Lei WB, et al. Clinical characteristics and endoscopic endonasal removal of foreign bodies within sinuses, orbit, and skull base. Chin Med J (Engl) 2017;130:1816-1823. https://doi.org/10.4103/0366-6999.211545
- Levin B, Goh ES, Ng YH, et al. Endoscopic removal of a foreign body in the orbital apex abutting the optic nerve. Singapore Med J 2019;60:265-266. https://doi.org/10.11622/smedj.2019045
- Bocchialini G, Negrini S, Bolzoni Villaret A, et al. Intraconal orbital displacement of a dental implant treated with an endoscopically-assisted approach. Br J Oral Maxillofac Surg 2020;58:469-471. https://doi.org/10.1016/j.bjoms.2020.01.006
- Sasindran V, John MS, Augustian SM. Removal of intraorbital foreign body by transnasal endoscopic approach. Indian J Otolaryngol Head Neck Surg 2023;75(Suppl 1):1090-1092. https://doi.org/10.1007/s12070-023-03596-6
- Hou YT, Wei YH, Liao CK, et al. Personalized multidisciplinary approach of orbital apex foreign body: a case report and literature review. Taiwan J Ophthalmol 2022;12:374-377. https://doi.org/10.4103/tjo.tjo_26_22
- Koo Ng NK, Jaberoo MC, Pulido M, et al. Image guidance removal of a foreign body in the orbital apex. Orbit 2009;28:404-407. https://doi.org/10.3109/01676830903074087
- Castelnuovo P, Turri-Zanoni M, Battaglia P, et al. Endoscopic endonasal management of orbital pathologies. Neurosurg Clin North Am 2015;26:463-472. https://doi.org/10.1016/j.nec.2015.03.001
- Castelnuovo P, Dallan I, Locatelli D, et al. Endoscopic transnasal intraorbital surgery: our experience with 16 cases. Eur Arch Otorhinolaryngol 2012;269:1929-1935. https://doi.org/10.1007/s00405-011-1917-z
- Sieskiewicz A, Lyson T, Mariak Z, et al. Endoscopic trans-nasal approach for biopsy of orbital tumours using image-guided neuro-navigation system. Acta Neurochir (Wien) 2008;150:441-445. https://doi.org/10.1007/s00701-008-1558-1
- Zoli M, Sollini G, Martinoni M, et al. Intra-operative ultrasonography in endoscopic approaches for orbital lesions: a single-center case series. Oper Neurosurg 2023;24:23-32. https://doi.org/10.1227/ons.0000000000000437
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2024 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 868 times
- PDF downloaded - 193 times




